Vaccine Supply Chain: How Vaccines Move from Lab to Your Arm
When you get a vaccine, it didn’t just appear in the clinic—it traveled through a complex vaccine supply chain, the end-to-end system that moves vaccines from manufacturing to the person being immunized. Also known as immunization logistics, it’s not just about shipping boxes—it’s about keeping vaccines alive. One degree too warm, one delay too long, and a dose can go bad. This isn’t theoretical. In 2021, over 1.5 million COVID-19 vaccine doses were discarded globally because of temperature failures. That’s not waste—it’s lost protection.
The cold chain logistics, the system of refrigerated transport and storage that maintains vaccines at precise temperatures is the backbone of this process. Some vaccines, like the original Pfizer-BioNTech COVID shot, need to be kept at -70°C. Others, like the Moderna or Johnson & Johnson shots, can survive in standard fridge temps. But even fridge-stable vaccines can’t sit out for hours. The vaccine distribution, the movement of vaccines across regions, countries, and clinics must be timed like a relay race. Each handoff—from factory to regional warehouse, to hospital freezer, to nurse’s cart—must happen without a break. Tracking systems use GPS and temperature sensors to flag problems before a dose is wasted. But in rural areas or conflict zones, these systems often don’t exist. That’s why some vaccines still arrive in coolers carried by motorbike or donkey.
The vaccine storage, how vaccines are kept before use, from large freezers to portable thermal boxes matters just as much as transport. A hospital might have a perfect freezer, but if the nurse leaves the vial on the counter while preparing shots, the heat can ruin it. That’s why training staff is part of the supply chain too. It’s not just about technology—it’s about people knowing what to do when the power goes out or the delivery is late. The vaccine supply chain isn’t glamorous, but it’s the reason millions stay healthy. When it works, you never notice it. When it fails, outbreaks follow.
What follows are real-world stories from the front lines: how temperature spikes killed batches, how logistics teams in remote villages kept vaccines alive, how packaging innovations changed the game, and why some countries get vaccines faster than others. These aren’t theory pieces—they’re lessons from the field. You’ll see how the same supply chain issues show up in flu shots, HPV vaccines, and childhood immunizations. No fluff. Just what works, what breaks, and what you need to know to understand why your shot arrived on time—or didn’t.
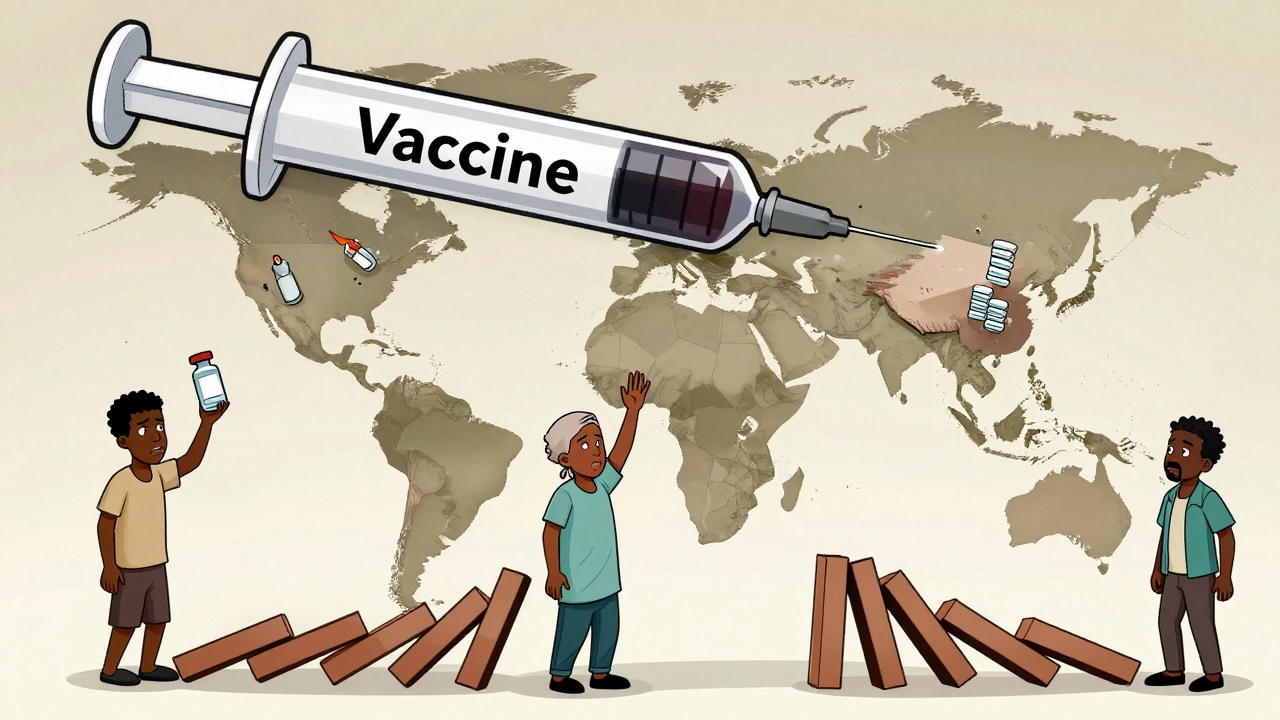
Vaccine Generics: Why Global Production and Access Remain Unequal
- Dec, 1 2025
- Daniel Remedios
- 11 Comments
Vaccine generics don't exist like regular drugs due to biological complexity. Global access remains unequal because of high costs, fragile supply chains, and patent barriers-leaving low-income countries dependent on imports.
