Vaccine Manufacturing: How Vaccines Are Made and Why It Matters
When you get a vaccine, you're not just getting protection—you're receiving the result of a complex, high-stakes process called vaccine manufacturing, the end-to-end process of developing, producing, and testing vaccines to ensure they’re safe and effective. Also known as vaccine production, it’s not like making pills or syrups. It’s a biological engineering feat that requires sterile labs, precise timing, and strict oversight at every step.
Behind every successful vaccine is a system built on quality assurance units, independent teams that verify each batch meets safety standards before release. These units must stay separate from production teams—because if the people making the vaccine also check it, mistakes slip through. The FDA and global health agencies require this separation for a reason: one error can cost lives. This isn’t theory. In the past, contaminated batches led to paralysis, infections, and deaths. That’s why today’s systems are designed to catch problems before they leave the facility. GMP compliance, the set of rules that govern how pharmaceutical products are made and tested, is the backbone of this process. It covers everything from how raw materials are stored to how workers wash their hands. Skipping a single GMP step can invalidate an entire production run.
But vaccine manufacturing doesn’t stop at cleanliness. It’s also about consistency. One batch must behave exactly like the next. That’s why every step—from growing viruses in chicken eggs or cell cultures to purifying proteins and filling vials—is monitored with sensors, logs, and automated checks. Even small changes in temperature or pH can ruin a batch. And unlike regular drugs, vaccines can’t be tested for effectiveness on every single unit. Instead, manufacturers rely on statistical sampling and proven protocols to guarantee safety. That’s why independent oversight isn’t just a best practice—it’s legally required. When quality assurance fails, the consequences ripple out: public trust erodes, vaccination rates drop, and outbreaks return. That’s why the posts below dive into the real-world details—how labs prevent contamination, why some vaccines need cold chains, and how regulators catch hidden flaws before they reach you.
What you’ll find here aren’t abstract theories. These are real stories from the factory floor and inspection room: how a single mislabeled vial nearly caused a recall, why certain antibiotics can’t be used near vaccine production, and how modern tech is making the whole process faster without cutting corners. This is the hidden science that keeps you safe—and it’s more fragile than you think.
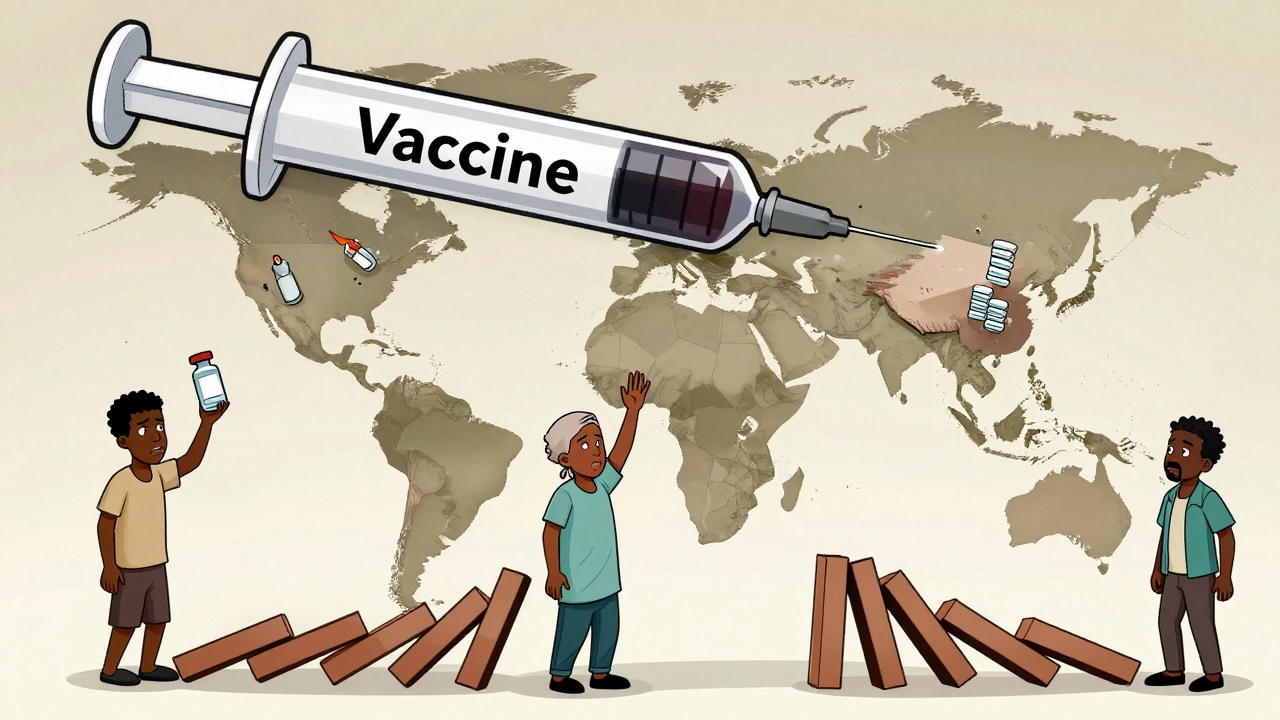
Vaccine Generics: Why Global Production and Access Remain Unequal
- Dec, 1 2025
- Daniel Remedios
- 11 Comments
Vaccine generics don't exist like regular drugs due to biological complexity. Global access remains unequal because of high costs, fragile supply chains, and patent barriers-leaving low-income countries dependent on imports.
