Radioactive Iodine: What It Is, How It’s Used, and What You Need to Know
When your thyroid goes haywire—whether it’s overactive, enlarged, or cancerous—radioactive iodine, a targeted form of radiation therapy that destroys thyroid tissue without surgery. Also known as iodine-131, it’s one of the most precise tools in nuclear medicine because the thyroid naturally pulls in iodine like a magnet. You swallow it as a pill or liquid, and within days, it homes in on thyroid cells, zapping abnormal ones while leaving the rest of your body mostly untouched.
This isn’t just for thyroid cancer. Many people with hyperthyroidism, a condition where the thyroid produces too much hormone get radioactive iodine because it’s more effective than long-term drugs and avoids the risks of surgery. It’s also the go-to after thyroid removal to kill off any leftover cancer cells. But it’s not magic—it comes with rules. You’ll need to avoid close contact with others for a few days, especially kids and pregnant women, because your body briefly emits radiation. And yes, it often leads to hypothyroidism, which means you’ll likely need to take thyroid hormone pills for the rest of your life. That’s not a side effect—it’s the point.
People often confuse radioactive iodine with regular iodine supplements or contrast dyes used in scans. They’re not the same. iodine-131, the specific isotope used in treatment, has a half-life of about eight days, meaning it fades quickly. Other forms like iodine-123 are used only for imaging, not treatment. And unlike chemotherapy, which floods your whole system, this treatment is local. It doesn’t cause hair loss or nausea unless you’re exposed to very high doses over time.
What you won’t find in most brochures? The real-world trade-offs. Some people feel fine after treatment. Others get a sore throat, dry mouth, or changes in taste for weeks. If you’re planning to get pregnant, you’ll need to wait at least six months—sometimes longer. And if you’re on thyroid meds already, your doctor will likely stop them for a few weeks before treatment so your thyroid cells are hungry enough to soak up the radioactive iodine. It’s not pleasant, but it’s proven. Studies show over 90% of thyroid cancer patients treated with it survive at least five years, often with no further treatment needed.
There’s no one-size-fits-all plan. Your age, cancer stage, thyroid size, and even your job (if you work with kids or in healthcare) all affect how the treatment is given. Some people need one dose. Others need two or three. And while it’s common, it’s not automatic. Many doctors now prefer to monitor small thyroid cancers instead of rushing to radiation—especially in older adults.
Below, you’ll find real-life guides on how to manage life after radioactive iodine treatment, what to expect during isolation, how to protect your family, and what other medications might interfere with it. You’ll also see how it compares to surgery, what the long-term risks really are, and why some people end up needing more than one round. This isn’t theory—it’s what people actually deal with after the pill is swallowed and the countdown begins.
Graves' Disease: Causes, Symptoms, and Proven Treatment Options for Autoimmune Hyperthyroidism
- Dec, 4 2025
- Daniel Remedios
- 14 Comments
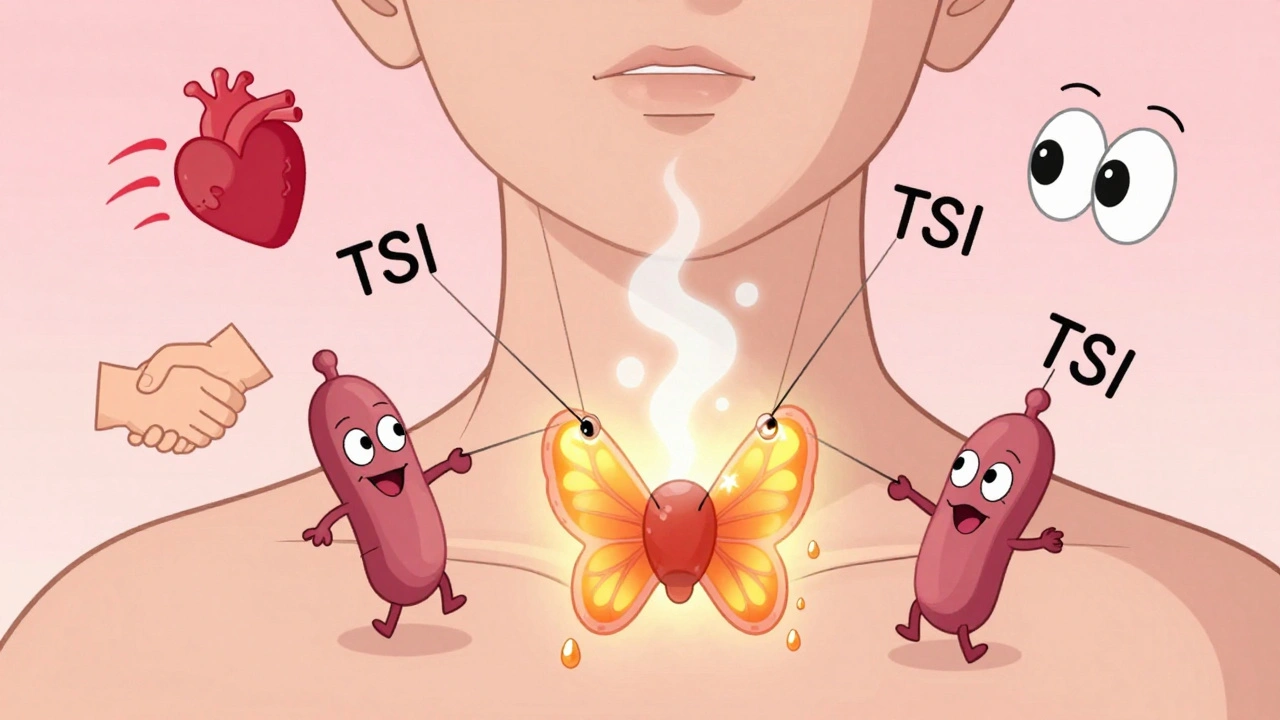
Graves' disease is the most common cause of hyperthyroidism, triggered by autoimmune antibodies that overstimulate the thyroid. Learn the symptoms, diagnostic tests, and proven treatments including medication, radioactive iodine, and surgery.
