Graves' disease is the most common cause of hyperthyroidism, affecting up to 90% of people with an overactive thyroid in countries with enough iodine in their diet. It’s not just a thyroid problem-it’s an autoimmune disorder where your immune system mistakenly attacks your own thyroid gland, forcing it to make too much hormone. This leads to a cascade of symptoms that can feel overwhelming: racing heart, unexplained weight loss, shaking hands, anxiety, and even bulging eyes. The good news? We know exactly how to diagnose it, and there are clear, effective treatments that work for most people.
How Graves’ Disease Actually Works
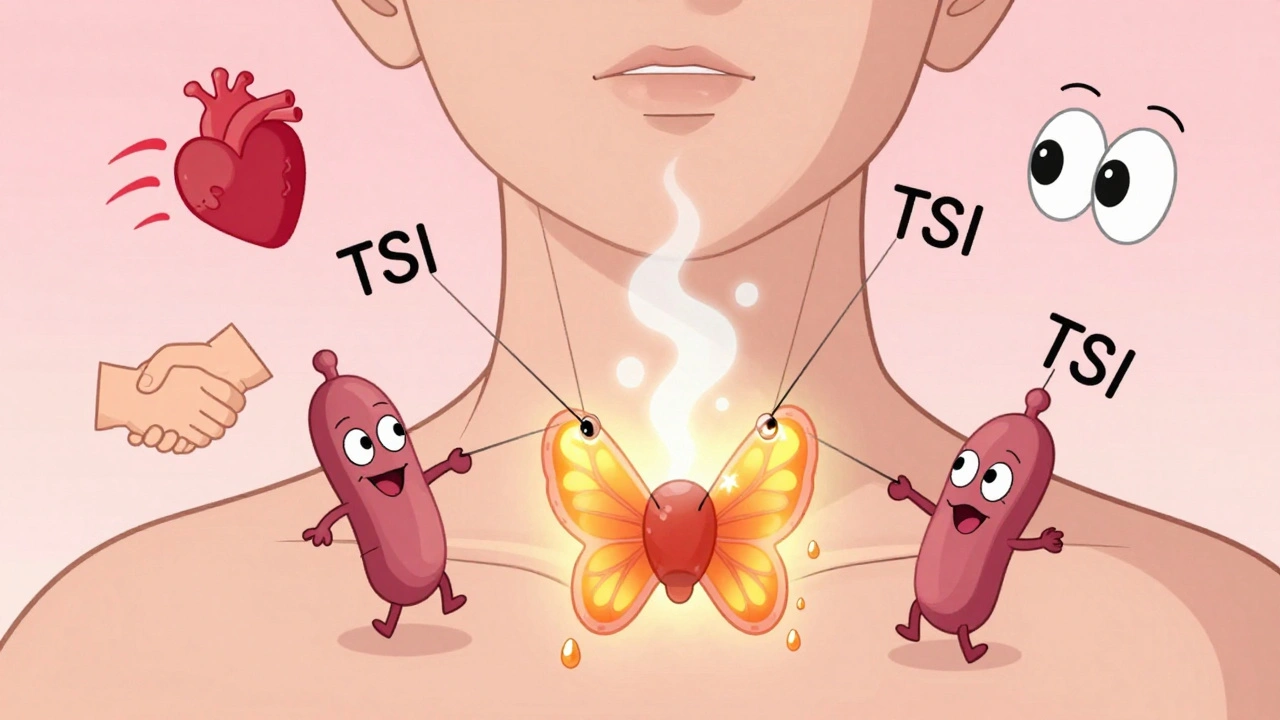
Your thyroid is a small butterfly-shaped gland in your neck that controls your metabolism. Normally, it responds to signals from your brain-specifically, a hormone called TSH. But in Graves’ disease, your body makes abnormal antibodies called thyroid-stimulating immunoglobulins (TSI). These antibodies act like fake TSH, tricking your thyroid into overproducing hormones no matter what your brain says. This isn’t random. Women are 7 to 8 times more likely to get it than men, and it usually shows up between ages 30 and 50. If someone in your family has an autoimmune disease-like type 1 diabetes, lupus, or rheumatoid arthritis-your risk goes up. Smoking also doubles or triples your chance of developing the eye complications linked to Graves’ disease. It’s not just about the thyroid; it’s about your whole immune system going off track.What Symptoms to Watch For
Symptoms vary by age and how long the disease has been active. Younger people often feel the most dramatic effects: anxiety, trouble sleeping, heart palpitations, and sudden weight loss even when eating more. You might sweat more than usual, feel hot when others are cold, or notice your hands trembling when you hold a cup. Fatigue is common, but so is muscle weakness-especially in your hips and shoulders. Bowel movements can become more frequent, and you might feel restless or irritable for no clear reason. Older adults, especially over 60, don’t always show these classic signs. Instead, they might feel unusually tired, have a fast or irregular heartbeat, or experience chest discomfort. Memory issues and confusion can be mistaken for aging, but they’re actually signs of too much thyroid hormone. About one in three people with Graves’ disease develop eye problems. This is called Graves’ ophthalmopathy. Eyes may bulge outward, feel dry or gritty, water excessively, or double vision can occur. In rare cases, vision can be threatened. A less common but still possible sign is pretibial myxedema-a thickening of the skin on the shins that looks like orange peel. These symptoms don’t always match how severe the thyroid overactivity is, which is why doctors look beyond just hormone levels.How Doctors Diagnose It
Diagnosis starts with a simple blood test. If your TSH is very low-under 0.4 mIU/L-and your free T4 and T3 levels are high, that’s a strong red flag. But to confirm it’s Graves’ disease and not another cause of hyperthyroidism, doctors test for specific antibodies. TSI and TRAb (TSH receptor antibodies) are present in 85-95% of people with Graves’. If these are positive, no further tests are usually needed. If antibody tests aren’t available, a radioactive iodine uptake scan can help. In Graves’ disease, the thyroid soaks up iodine like a sponge, showing a smooth, full uptake across the whole gland. Other causes, like thyroid nodules, show patchy uptake. Ultrasound can also detect increased blood flow in the thyroid, which is another hallmark of Graves’. Your doctor will also ask about your family history, recent stress, pregnancy (which can trigger the disease), and whether you smoke. Smoking isn’t just a bad habit here-it’s a major risk factor for severe eye disease. If you smoke and have Graves’, quitting is the single most important thing you can do to protect your eyes.
Three Main Treatment Paths
There are three approved ways to treat Graves’ disease: medication, radioactive iodine, and surgery. Each has pros and cons, and the right choice depends on your age, symptoms, preferences, and whether you have eye problems. Antithyroid drugs like methimazole or propylthiouracil block the thyroid from making extra hormone. Methimazole is usually preferred because it’s safer-propylthiouracil carries a small risk of liver damage. You typically start with a higher dose, then lower it once hormone levels normalize. Most people take these for 12 to 18 months. About 30-50% go into remission after that time, meaning the disease stays quiet without more treatment. The chances of remission are higher if your thyroid is only slightly enlarged and your antibody levels drop to zero before stopping the medication. Radioactive iodine (I-131) is the most common treatment in the U.S. You swallow a pill or liquid containing a small dose of radioactive iodine. The thyroid absorbs it like regular iodine, and the radiation slowly destroys the overactive cells. Within 6 to 12 months, most people become hypothyroid-meaning their thyroid stops working entirely. That sounds scary, but it’s easily managed with daily levothyroxine, a simple pill that replaces the missing hormone. The big advantage? It’s a one-time treatment with no surgery. The downside? You’ll need thyroid medication for life. Surgery (thyroidectomy) removes all or part of the thyroid. It’s usually reserved for people with very large goiters that cause trouble swallowing or breathing, those who can’t take antithyroid drugs or radioactive iodine, or those with severe eye disease. Success rates are over 95%, but there are risks: damage to the vocal cords (less than 1%) or the parathyroid glands (1-2%), which control calcium levels. After surgery, you’ll also need lifelong thyroid hormone replacement.Treating the Eyes: More Than Just a Side Effect
Graves’ eye disease doesn’t always improve when the thyroid is under control. That’s why it needs its own treatment plan. For mild cases, selenium supplements (100 mcg twice daily for 6 months) can reduce swelling and discomfort. For moderate to severe cases, doctors use high-dose IV steroids like methylprednisolone. A typical course is 500 mg once a week for 6 weeks, then 250 mg for another 6 weeks. About 60-70% of patients see noticeable improvement. If steroids don’t work or the eye bulging is severe, a newer drug called teprotumumab is changing the game. It targets a receptor involved in eye tissue swelling. In clinical trials, 75-80% of patients had a major reduction in eye bulging after 24 weeks-compared to only 20% in the placebo group. This is now an FDA-approved option for moderate-to-severe cases. In extreme cases where vision is at risk, orbital decompression surgery can remove bone around the eye socket to give the eyeball more space. This is often the last resort but can restore normal appearance and vision after months or years of discomfort.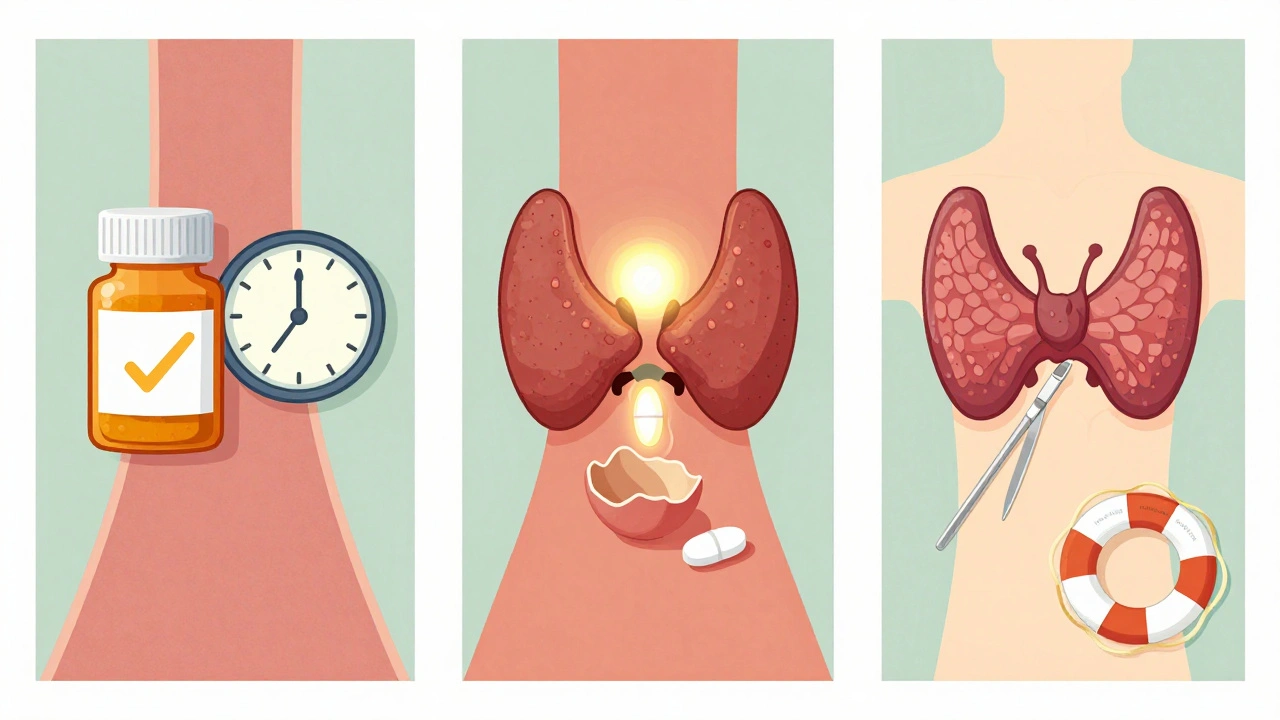

Ada Maklagina
I had Graves' in my 30s. Took methimazole for 18 months, went into remission. No more bulging eyes, no more heart racing at 3am. Just took a deep breath and lived.
Still take selenium every day. Small thing, big difference.
Michael Dioso
They say radioactive iodine is the most common treatment in the US. Funny how that's also the same place where they sell detox teas and sell your blood for crypto.
Krishan Patel
You people treat this like a medical condition when it's clearly a spiritual imbalance. Your immune system is screaming because you're disconnected from your ancestors, glued to screens, and eating processed garbage. No pill fixes that. Quit blaming your thyroid and start fixing your soul.
Norene Fulwiler
My mom had this. She quit smoking cold turkey after diagnosis and her eye swelling went down in weeks. No magic, just discipline. If you're smoking and have Graves', you're not just risking your eyes-you're risking your future.
sean whitfield
Teprotumumab? Sounds like a pharmaceutical deep state product. They invented a $100k drug for eyes so they can keep you hooked on biologics. Meanwhile, the real cure is sunlight, fasting, and silence.
aditya dixit
I've seen patients come in terrified of lifelong meds after RAI. But here's the truth: you're not losing your thyroid-you're gaining control. Levothyroxine is simple. It's not a life sentence, it's a life upgrade. You get to sleep. You get to eat. You get to breathe. That's not a tragedy. That's peace.
Lucy Kavanagh
They never tell you the government knows about this. Thyroid disorders spiked right after fluoridation started. Coincidence? Or is your water secretly weaponized? I’ve got 7 friends with Graves' and all of them drank tap water since birth.
Chris Brown
I find it deeply concerning that so many people accept radioactive iodine as a standard of care. This is not a solution. It is an abandonment of the body's inherent wisdom. We are treating symptoms, not restoring harmony. The medical industrial complex profits from chronicity.
Stephanie Fiero
Just wanted to say i took methimazole and got a rash and thought i was gonna die. went to er and they said its common. i was scared but kept going. 2 years later im fine. dont give up. its hard but you got this.
Laura Saye
There's a profound metaphysical layer here. The thyroid governs expression, communication, the voice. When it's hijacked, it's not just hormones-it's the soul's cry for boundaries. You're not overproducing T3. You're overproducing the need to be heard. Healing begins when you stop swallowing your truth.
Mark Curry
i had this too. took the iodine. now i take my little pill every morning. its fine. just remember to take it on empty stomach. and dont drink coffee right after. lol. peace out 🌞
luke newton
You think this is just about your thyroid? Wake up. It’s the toxins. The plastics. The EMFs. The glyphosate in your oat milk. Your body isn't broken-it's trying to detox. And they want you to believe a pill fixes it so you never question the system.
Lynette Myles
TSI antibodies positive? Then you’re not getting better until you stop gluten.
William Chin
I appreciate the comprehensive overview. However, I must emphasize that the omission of any mention of the role of chronic psychological stress as a primary precipitating factor in autoimmune dysregulation constitutes a significant lacuna in the clinical narrative. One cannot treat the gland without addressing the mind.