Platelet Drop: Causes, Risks, and What to Do When Your Blood Count Falls
When your platelet drop, a sudden or sustained decrease in the number of blood cells that help your blood clot. Also known as thrombocytopenia, it can turn a small cut into a serious problem—or cause bleeding you didn’t even notice. Platelets are tiny, but they’re your body’s first responders to injury. If your count falls below 150,000 per microliter, you’re in the red zone. Below 50,000, even brushing your teeth might leave you bruised. Below 20,000, you’re at real risk of internal bleeding.
A platelet drop, a sudden or sustained decrease in the number of blood cells that help your blood clot. Also known as thrombocytopenia, it can turn a small cut into a serious problem—or cause bleeding you didn’t even notice. Platelets are tiny, but they’re your body’s first responders to injury. If your count falls below 150,000 per microliter, you’re in the red zone. Below 50,000, even brushing your teeth might leave you bruised. Below 20,000, you’re at real risk of internal bleeding.
Many things cause this. Some are harmless—like a viral infection that knocks your platelets down for a week or two. Others are serious. Certain antibiotics, chemotherapy, or even heavy alcohol use can shut down your bone marrow’s ability to make them. Autoimmune diseases like ITP force your immune system to attack your own platelets. And some drugs, like heparin, can trigger a rare but dangerous reaction called HIT, where your body destroys platelets instead of using them to clot.
It’s not just about the number. It’s about what’s behind it. If your platelet drop came after starting a new medication, that’s a red flag. If you’re also losing red blood cells or white cells, it could point to something deeper—like leukemia or bone marrow failure. And if you’re on blood thinners or dual antiplatelet therapy after a stent, a sudden drop could mean internal bleeding you didn’t feel yet.
You don’t always feel it. But signs show up: tiny red dots on your skin (petechiae), nosebleeds that won’t stop, gums that bleed for no reason, or unusually heavy periods. Women often notice it first. Men might see it after a fall or surgery. Older adults are more at risk because their bone marrow slows down naturally, and they’re more likely to be on meds that affect platelets.
What you do next matters. Don’t ignore it. A simple blood test can confirm it. But then you need to find out why. That means talking to your doctor about every pill you take—even the herbal ones. Some supplements, like fish oil or high-dose vitamin E, thin your blood and can make a platelet drop worse. And if you’re already on warfarin or NSAIDs, the combo can be dangerous.
There’s no one fix. Sometimes, you just wait. Other times, you stop a drug, start steroids, or get a platelet transfusion. But the key is catching it early. The longer you wait, the more damage can happen inside your body—without you knowing.
In the articles below, you’ll find real cases and clear advice on what causes platelet drop, how to spot it before it’s too late, which medications can trigger it, and what steps you can take to protect yourself—whether you’re managing a chronic condition, recovering from surgery, or just wondering why you’re bruising so easily.
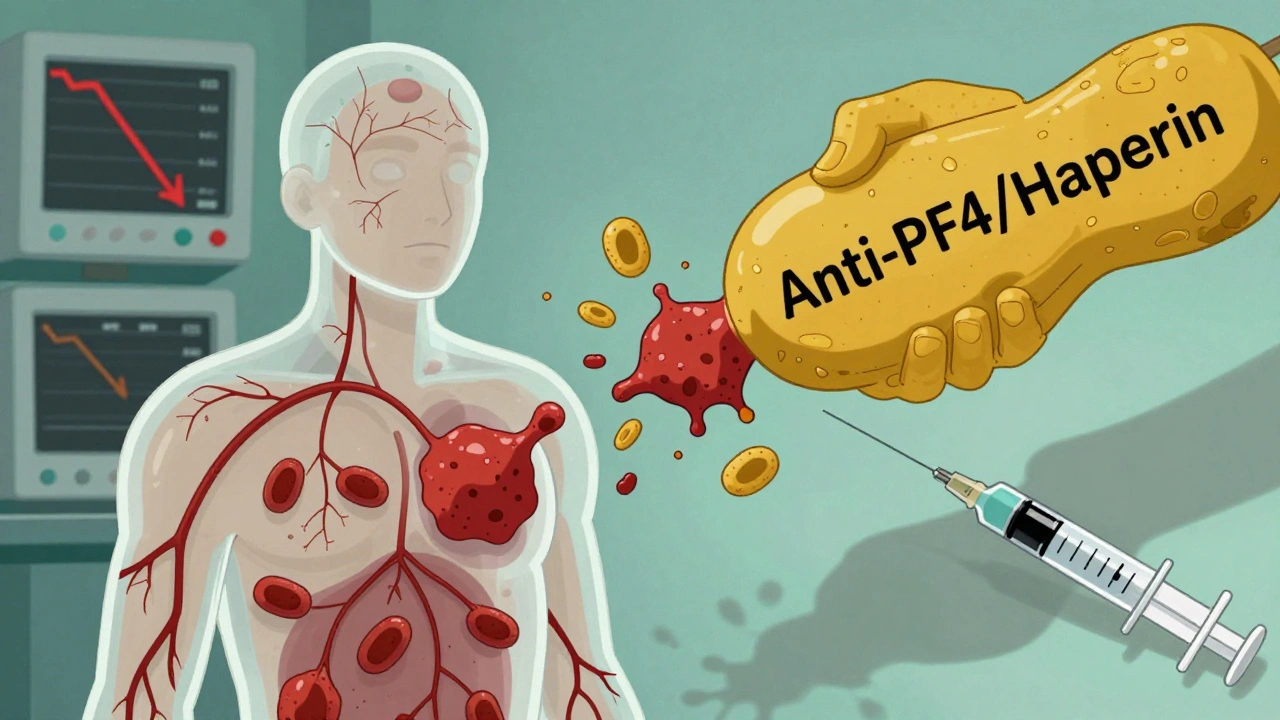
Heparin-Induced Thrombocytopenia: What You Need to Know About This Rare but Dangerous Side Effect
- Dec, 5 2025
- Daniel Remedios
- 11 Comments
Heparin-induced thrombocytopenia (HIT) is a rare but life-threatening reaction to heparin that causes low platelets and dangerous blood clots. Learn the signs, who’s at risk, and what to do if it happens.
