Pheochromocytoma – What It Is and Why It Matters
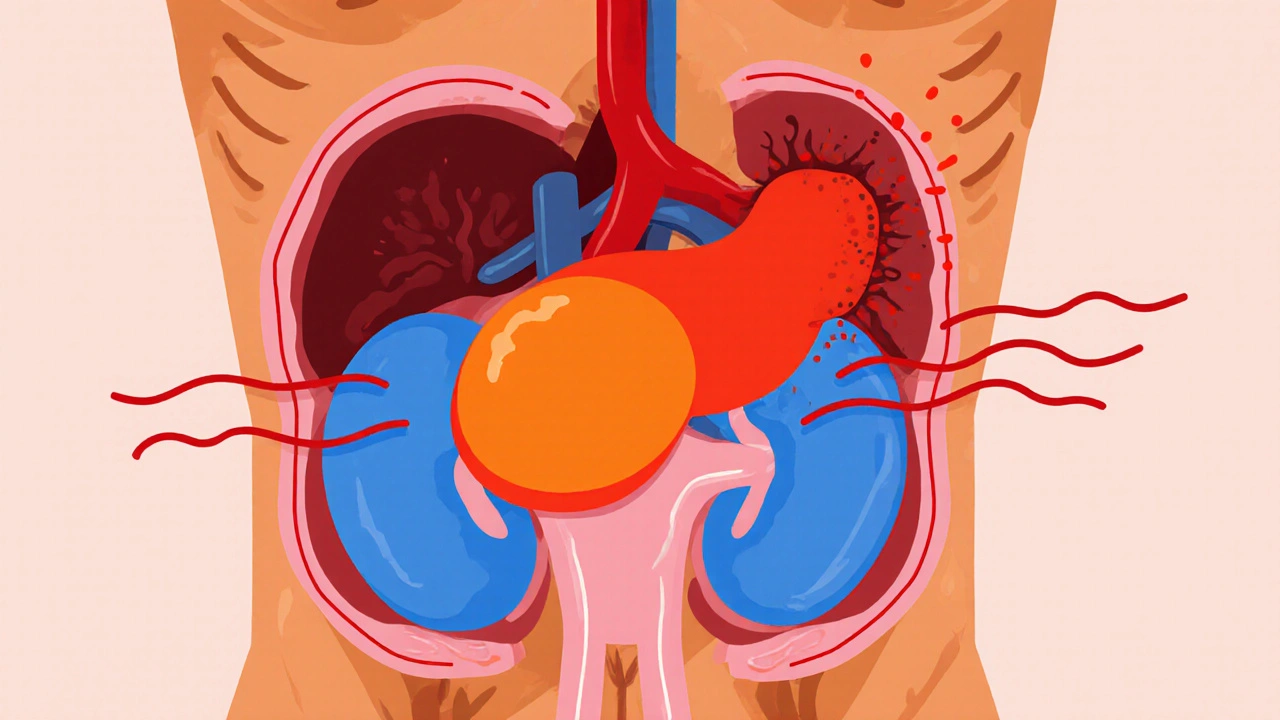
When working with pheochromocytoma, a rare tumor that grows in the adrenal medulla and releases large amounts of catecholamines. Also known as adrenal pheochromocytoma, it can trigger sudden spikes in blood pressure and cause a range of symptoms that often catch people off guard.
One of the most common signs of pheochromocytoma is persistent or episodic hypertension, high blood pressure that can suddenly rise. The tumor pours out catecholamines, hormones like adrenaline and noradrenaline that regulate heart rate and blood vessels, which explains the pounding heart, sweating, and panic‑like episodes many patients describe. In short, pheochromocytoma triggers hypertension by flooding the bloodstream with catecholamines.
Diagnosing the condition usually starts with biochemical testing. Doctors check plasma‑free metanephrines or urinary catecholamine levels because elevated numbers flag the tumor’s activity. Imaging then steps in: a contrast‑enhanced CT scan, computed tomography that visualizes the adrenal region or an MRI, magnetic resonance imaging that offers detailed soft‑tissue contrast can locate the growth. For tricky cases, a specialized MIBG scan, a nuclear medicine test that highlights catecholamine‑producing tissue may be ordered. These steps together create a reliable picture of where the tumor lives and how active it is.
Treatment hinges on two goals: control the hormone surge and remove the tumor. Most patients start with an alpha‑blocker, medication that relaxes blood vessels and lowers blood pressure to keep symptoms in check before surgery. Once the blood pressure is stable, surgeons perform a laparoscopic adrenalectomy, which is often curative. In some hereditary cases, doctors may also consider a beta‑blocker, drug that slows the heart after alpha‑blockade to protect against heart rhythm problems. Effective treatment often requires surgical removal of the adrenal tumor, followed by lifelong follow‑up to catch any recurrence early.
Up to 40% of cases involve genetic mutations, changes in genes such as RET, VHL, or NF1 that increase tumor risk. Because of this, genetic counseling is recommended for patients and their families. Identifying a hereditary link can guide screening for relatives and influence the choice of surveillance imaging. It also shapes the conversation about future pregnancies, as some mutations can be passed to children.
Living with pheochromocytoma doesn’t end at surgery. Regular blood pressure monitoring, periodic biochemical tests, and occasional imaging keep the condition in check. Many patients also benefit from lifestyle tweaks: limiting caffeine, managing stress, and staying hydrated can reduce adrenaline surges. A multidisciplinary team—endocrinologist, surgeon, geneticist, and primary care doctor—helps tailor a plan that fits each person’s risks and goals.
What You’ll Find Below
Below you’ll discover a curated set of articles that dive deeper into each piece of this puzzle: symptom checklists, medication comparisons, imaging guides, and genetic testing advice. Whether you’re looking for practical tips to manage blood pressure spikes or want to understand the science behind catecholamine excess, the posts ahead give clear, actionable information.
Pheochromocytoma: New Research & Treatment Advances 2025
- Oct, 18 2025
- Daniel Remedios
- 15 Comments
A concise guide on pheochromocytoma covering new genetic insights, modern diagnostics, treatment options from surgery to radiotherapy, and emerging therapies in 2025.
