INR Monitoring: What It Is, Why It Matters, and What You Need to Know
When you're on a blood thinner like warfarin, a common anticoagulant used to prevent dangerous blood clots. Also known as Coumadin, it works by slowing down your body’s clotting process. But too much can cause uncontrolled bleeding, and too little leaves you at risk for stroke or heart attack. That’s where INR monitoring, a simple blood test that measures how long it takes your blood to clot comes in. It’s not just a number—it’s your safety net.
INR stands for International Normalized Ratio. It’s the standard way doctors track how well your blood is thinning. A normal INR for someone not on blood thinners is around 1.0. But if you have a mechanical heart valve, atrial fibrillation, or a history of clots, your target might be between 2.0 and 3.5. Too low? You’re not protected enough. Too high? You’re one fall or cut away from serious bleeding. That’s why regular checks matter. People on warfarin often get tested every week at first, then maybe every few weeks once things stabilize. But even small changes—like eating more greens, starting a new antibiotic, or skipping a dose—can throw your INR off. That’s why it’s not just about the test. It’s about understanding what affects it.
INR monitoring doesn’t exist in a vacuum. It connects to other things you might be taking. For example, acid-reducing medications, like proton pump inhibitors, can interfere with how warfarin is absorbed. Some antibiotics and even herbal supplements like St. John’s wort can make your INR swing unpredictably. And if you’re on dual antiplatelet therapy, like aspirin plus clopidogrel after a stent, your bleeding risk multiplies. Your INR might be fine, but your overall clotting balance is more fragile. That’s why knowing your full medication list is just as important as the test result.
You might not think of INR when you’re dealing with something like tinnitus or stomach pain, but if you’re on blood thinners, those issues can become more serious. A head injury? Even a mild one could lead to internal bleeding. A stomach ulcer? It could bleed out without warning. That’s why people on anticoagulants need to be extra careful with pain relievers—aspirin is risky, acetaminophen is safer. And if you’re traveling across time zones or changing your diet, your INR can shift. It’s not just a lab result. It’s a daily balancing act.
Below, you’ll find real-world guides on how medications interact, how to spot dangerous side effects, and what to do when things go off track. Whether you’re new to INR monitoring or you’ve been doing it for years, these posts give you the practical, no-fluff info you need to stay safe and in control.
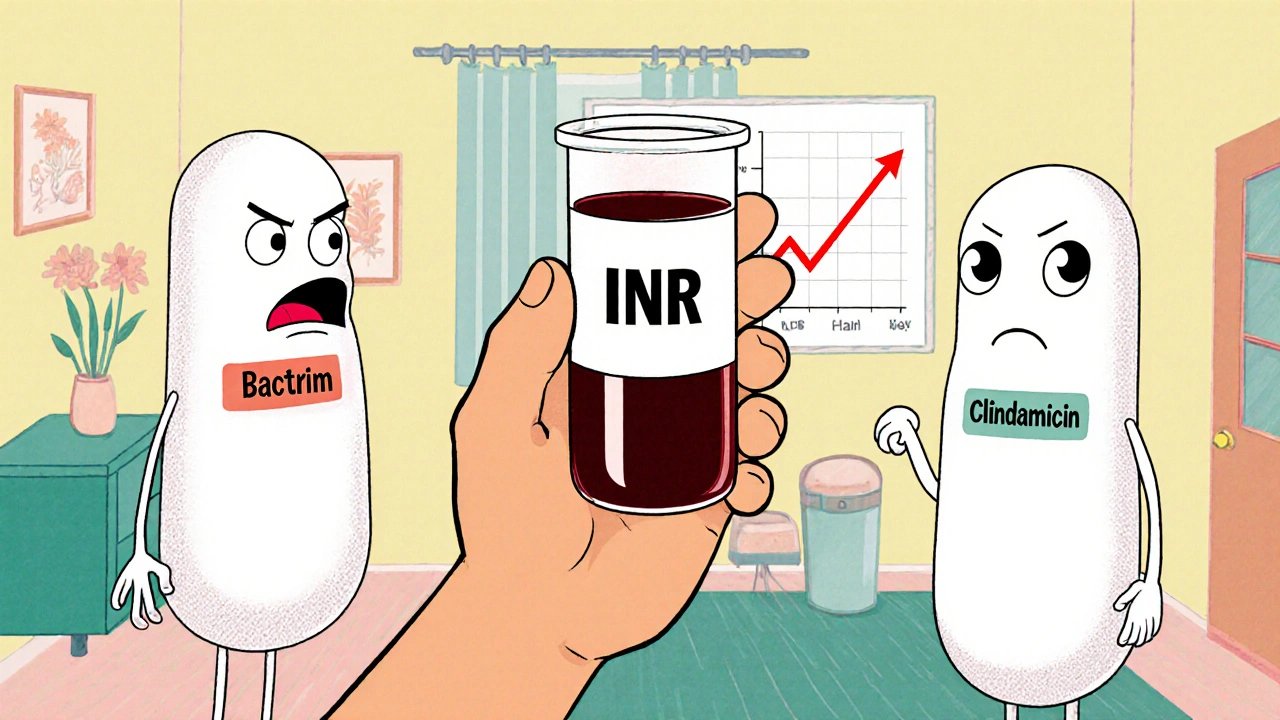
Managing Warfarin and Antibiotics: What You Need to Know About Dangerous Interactions
- Nov, 13 2025
- Daniel Remedios
- 14 Comments
Warfarin and antibiotics can interact dangerously, raising bleeding risk or reducing effectiveness. Learn which antibiotics are high-risk, when to check your INR, and how to stay safe without stopping treatment.
