Acid-Reducing Medications: What They Are, How They Work, and What You Need to Know
When your stomach makes too much acid, it can burn your esophagus, cause chronic heartburn, or even lead to ulcers. Acid-reducing medications, a category of drugs designed to lower stomach acid production or neutralize it. Also known as antacids, H2 blockers, or proton pump inhibitors, these are among the most commonly used drugs worldwide for digestive discomfort. But not all acid-reducing meds are the same—and using them wrong can cause more harm than good.
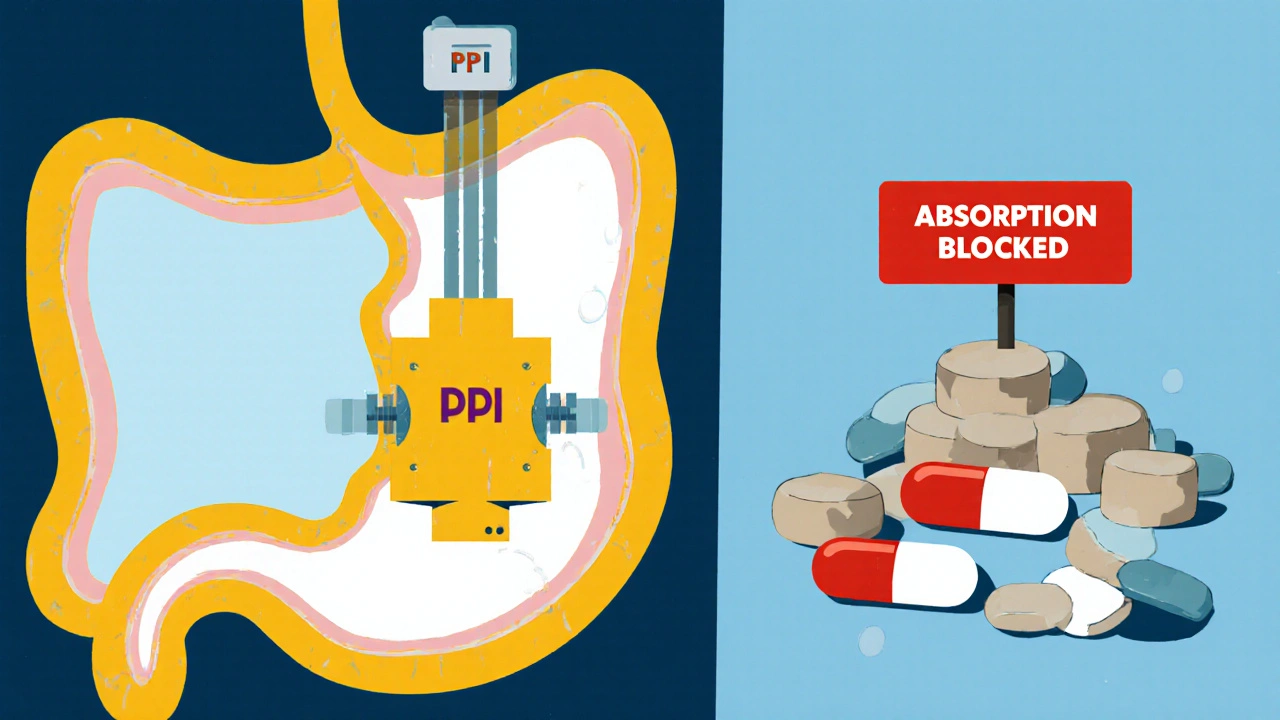
Two main types dominate the market: proton pump inhibitors (PPIs), drugs like omeprazole and esomeprazole that shut down acid-producing pumps in the stomach lining, and H2 blockers, such as ranitidine and famotidine, which reduce acid by blocking histamine receptors. PPIs are stronger and longer-lasting, often prescribed for GERD or ulcers. H2 blockers work faster but don’t last as long, making them better for occasional heartburn. But here’s the catch: long-term PPI use has been linked to nutrient deficiencies, bone loss, and even kidney issues. That’s why doctors now recommend the lowest effective dose for the shortest time possible.
Many people don’t realize that acid reflux isn’t always caused by too much acid. Sometimes, it’s a weak lower esophageal sphincter letting acid creep up—no matter how much you reduce stomach acid. That’s why some folks keep having symptoms even while taking PPIs. The real fix? Lifestyle changes: losing weight, avoiding late-night meals, cutting out spicy or fatty foods, and not lying down right after eating. These aren’t just "tips"—they’re backed by studies showing they can reduce or even eliminate symptoms without drugs.
And then there’s the hidden problem: overuse. Millions take these meds daily without ever being re-evaluated. If you’ve been on a PPI for more than a year, ask your doctor if you still need it. Some people can taper off safely. Others need a different approach—like switching to an H2 blocker or using it only when symptoms flare. And if your heartburn is tied to something like Zollinger-Ellison syndrome, you need a totally different plan, one that targets the root cause, not just the symptom.
The posts below cover real-world cases: how simethicone helps with bloating after meals, why warfarin and acid meds can clash, how metoclopramide can replace some acid reducers for gastroparesis, and why Zollinger-Ellison syndrome increases osteoporosis risk. You’ll find comparisons, safety tips, and alternatives—not just marketing claims. This isn’t about selling you a pill. It’s about helping you understand what’s really going on in your gut—and what you can do about it.
Acid-Reducing Medications: How They Interfere with Other Drugs
- Nov, 17 2025
- Daniel Remedios
- 12 Comments
Acid-reducing medications like PPIs and H2 blockers can severely reduce the absorption of critical drugs including HIV, cancer, and antifungal treatments. Learn which medications are affected, why it happens, and how to protect your treatment.
