When your doctor prescribes a medication, you might see a brand name like Lipitor, Coumadin, or Allegra on the prescription. But when you pick it up at the pharmacy, the pill looks different - maybe a different color, shape, or label. You might wonder: Is this the same thing? Is it safe? Why would anyone switch?
The answer is simple: generic medications are just as effective as brand-name drugs, but they cost a fraction of the price. And millions of people are already making the switch - not because they have to, but because they can.
Generic drugs are not cheaper because they’re weaker
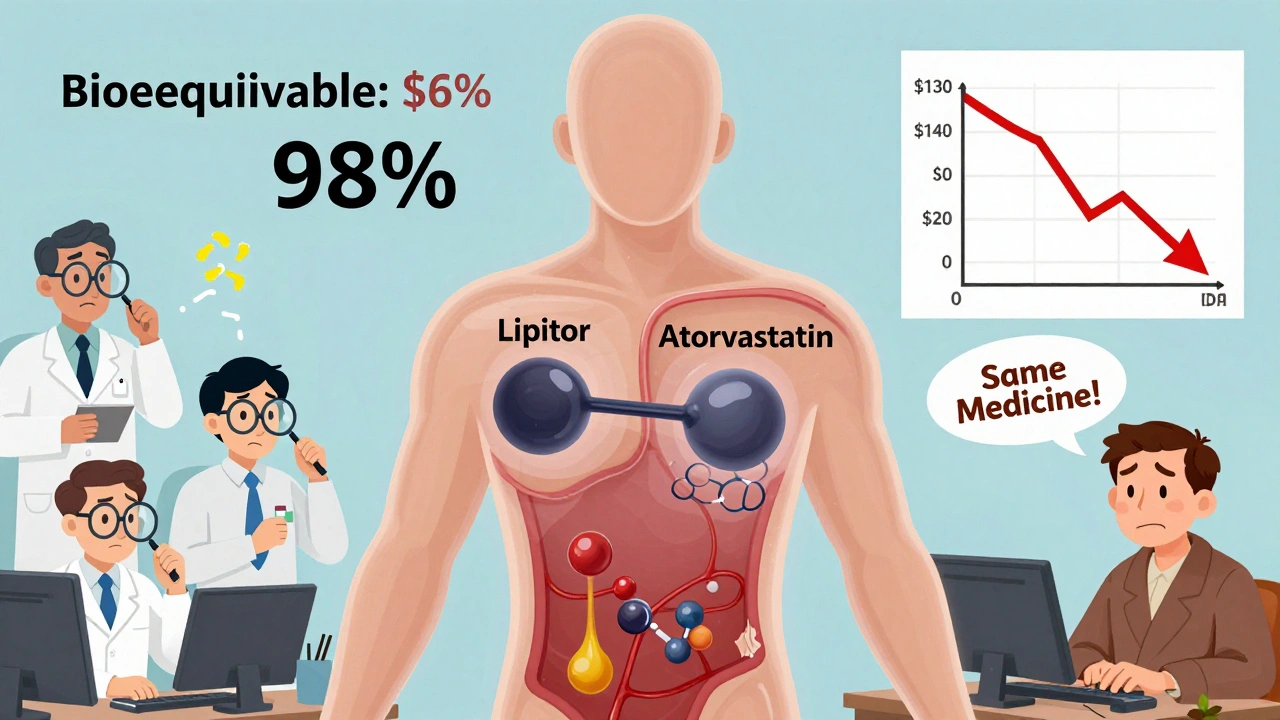
A lot of people assume that if a drug is cheaper, it must be lower quality. That’s not true. The U.S. Food and Drug Administration (FDA) requires generic drugs to have the same active ingredients, strength, dosage form, and route of administration as the brand-name version. That means if you’re taking a generic version of atorvastatin, it’s chemically identical to Lipitor. It works the same way in your body.
The FDA doesn’t just accept claims - they test. Before a generic drug hits the shelf, it must prove bioequivalence. That means the amount of medicine that enters your bloodstream and how fast it gets there must be within 80% to 125% of the brand-name drug. That’s not a guess. It’s science. And it’s required for every single generic approved in the U.S.
Even for drugs with narrow therapeutic windows - like blood thinners or seizure medications - the FDA holds generics to the same strict standards. While some doctors may monitor patients more closely when switching these types of drugs, studies show no meaningful difference in outcomes when generics are used properly.
How much money can you actually save?
Let’s talk numbers. The average generic drug costs 80% to 85% less than its brand-name counterpart. That’s not a small difference - it’s life-changing for many people.
Take warfarin, a blood thinner. The brand-name version, Coumadin, can cost over $300 for a 30-day supply. The generic? Around $4. That’s a 98% drop in price.
Or consider atorvastatin (Lipitor). When the patent expired in 2011, the brand-name version sold for about $130 a month. Today, the generic version is available for as little as $4 at major pharmacies. That’s not a sale. That’s a revolution.
Even common medications like metformin (for diabetes) or fexofenadine (for allergies) show the same pattern. Metformin generics cost $4 a month versus $300 for Glucophage. Fexofenadine generics run about $10, while Allegra costs $30.
And it’s not just individuals saving. In the last decade, generic drugs saved the U.S. healthcare system over $1.6 trillion. That’s money that goes back into hospitals, research, and patient care - not into corporate profits.
Insurance plans reward you for choosing generics
If you have insurance, your plan probably pushes you toward generics - and for good reason. Most insurance companies use tiered formularies. That means your copay is lowest for generics, higher for brand-name drugs, and highest for specialty medications.
With Humana, for example, the average copay for a generic is $1 to $10. For a brand-name drug? $25 to $75. That’s a difference of $65 a month - over $780 a year - just from switching.
Medicare Part D beneficiaries pay an average of $1.85 per generic prescription versus $33.67 for brand-name drugs. That’s not a typo. That’s the reality for millions of seniors.
And if you’re paying out of pocket? Many pharmacies offer $4 generic lists. You can get 30 days of high blood pressure, cholesterol, or diabetes meds for the price of a coffee.
Are generics as safe as brand-name drugs?
Safety is the biggest concern people have. And the data says: yes, they’re just as safe.
The FDA inspects over 1,200 manufacturing facilities each year - including those making generics - to ensure they meet the same quality standards as brand-name producers. In fact, many brand-name companies make their own generic versions under different labels.
Adverse event reports for generics are proportional to their usage. Since generics make up about 90% of all prescriptions, they naturally show up in more reports. But when you adjust for volume, the rate of side effects is identical to brand-name drugs.
A 2022 study of 186,000 heart patients found no difference in outcomes between those taking generic and brand-name cardiovascular drugs. Another study of 5,000 patients showed people using generics were 68% less likely to skip doses because of cost.
That’s huge. Skipping doses because you can’t afford your meds is a silent crisis. Switching to generics keeps people on treatment. That means fewer hospital visits, fewer complications, and better long-term health.
Why do generics look different?
Generic pills often look different because U.S. law requires them to be visually distinct from brand-name versions. That’s to avoid confusion - not because they’re different.
The differences are only in inactive ingredients: color, shape, flavor, or fillers. These don’t affect how the medicine works. But they can cause anxiety.
One patient on Drugs.com wrote: “My pill changed color and I panicked. I thought I got the wrong medicine.” Her doctor reassured her - it was the same drug, just made by a different company. She started saving $280 a month.
If you’re worried about a change in appearance, talk to your pharmacist. They can confirm it’s the same medication and explain why the look changed. Most pharmacies will even let you request a specific generic manufacturer if you prefer a certain look.
What about complex drugs? Are generics okay for those too?
Some drugs are harder to copy - like biologics, inhalers, or topical creams. These are called complex generics or biosimilars. But even these are being developed and approved.
As of December 2023, the FDA had approved 37 biosimilars - generic versions of expensive biologic drugs used for cancer, arthritis, and autoimmune diseases. These are not exact copies, but they’re proven to work just as well.
The Congressional Budget Office estimates biosimilars could save Medicare $50 billion a year by 2030. That’s not science fiction - it’s already happening.
And the FDA is working to remove barriers to generic entry for complex drugs like inhalers and eye drops. Their 2023 Drug Competition Action Plan is focused on making these drugs more affordable, faster.

What do doctors and experts say?
The American Medical Association recommends prescribing generics whenever appropriate. The FDA’s former director, Dr. Janet Woodcock, said: “Generic drugs undergo rigorous review to ensure they are as safe and effective as brand-name drugs.”
Harvard Medical School’s Dr. Aaron Kesselheim reviewed data from over 180,000 patients and concluded: “Our research confirms that generic cardiovascular drugs perform as well as their brand-name counterparts.”
Even in specialties like neurology, where some worry about seizure meds, experts agree: approved generics are safe. Dr. James Grogan of Mayo Clinic says, “For most patients, the switch is seamless. Only in rare cases do we need to monitor more closely.”
There’s no conspiracy. No cover-up. Just science, regulation, and economics working together to make medicine affordable.
How to switch - and what to watch for
Switching is easy. When your prescription is renewed, ask your pharmacist: “Is there a generic version?” They’ll tell you. If there is, and your doctor hasn’t blocked substitution, they’ll fill it automatically - unless you say otherwise.
If you’re nervous, ask your doctor to write “Dispense as Written” or “Brand Necessary” on the prescription. But only do that if you’ve had a real reaction to a generic in the past - not because you’re afraid.
Keep a list of your meds and their generic names. For example:
- Lipitor → atorvastatin
- Coumadin → warfarin
- Allegra → fexofenadine
- Glucophage → metformin
- Prilosec → omeprazole
Use the FDA’s Orange Book (online or through your pharmacist) to check therapeutic equivalence. It lists every approved generic and whether it’s rated as equivalent.
And if you notice any changes in how you feel after switching - fatigue, dizziness, new side effects - tell your doctor. But don’t assume it’s the generic. Sometimes, other factors are at play.
Bottom line: Switching saves money - without sacrificing health
There’s no reason to pay more for the same medicine. Generics are not second-rate. They’re not experimental. They’re FDA-approved, clinically proven, and widely used by millions.
Every time you choose a generic, you’re not just saving money. You’re keeping your treatment on track. You’re reducing stress about bills. You’re helping the system work better for everyone.
Ask your doctor or pharmacist about generics the next time you refill a prescription. You might be surprised how much you can save - and how little you’ll notice a difference.


Andrea DeWinter
So many people freak out when their pill changes color but don’t realize they’re saving hundreds a month
My grandma switched to generic metformin and now she’s got extra cash for her weekly bingo trips
She didn’t feel any different except way less stressed about bills
Nikhil Pattni
Bro I live in India and generics are literally the ONLY option here and let me tell you we don’t have FDA but we still get the same meds from same factories
Most brand name drugs in US are made in same plants as generics just different label
And yes I’ve taken generic atorvastatin for 5 years no issues
Also the FDA does inspect Indian plants too so stop thinking it’s some shady operation 😎
Andrea Petrov
Have you ever read the inactive ingredients list? Some generics use dyes that are banned in the EU
And don’t get me started on the fillers - I once had a reaction to a generic version that contained lactose
And no, my doctor didn’t warn me - because they don’t care about your allergies
It’s not about efficacy - it’s about corporate greed hiding behind FDA approval
They’re testing on us, not for us
And the fact that you’re so quick to trust the system? That’s the real problem.
Evelyn Pastrana
Generic meds = free money in your pocket
My cat’s meds cost more than my blood pressure pills
And I didn’t even notice the switch - until I checked my bank account
Also - if your pill looks different, that’s not a conspiracy
That’s just capitalism being weirdly helpful
Save your panic for actual emergencies like WiFi outages 😘
Arun Kumar Raut
I used to be scared of generics too until my dad had a heart attack
He was on brand name meds and couldn’t afford them
Switched to generic and he’s been stable for 8 years now
No side effects, no drama - just cheaper and works
Don’t let fear cost you your health
Ask your pharmacist - they’ll show you the science
It’s not magic, it’s just medicine
precious amzy
One must interrogate the epistemological foundations of pharmaceutical regulation.
The FDA, as a bureaucratic apparatus, operates within a neoliberal framework that commodifies health.
Generic equivalence is a statistical illusion - bioequivalence does not equal therapeutic equivalence.
One cannot reduce the human body to a pharmacokinetic model.
And yet, the masses are persuaded by the myth of ‘cost-efficiency’.
Is this not the ultimate triumph of instrumental reason over embodied experience?
One wonders - who benefits from this normalization?
Not the patient. Not the healer. Only the system.
Carina M
It is deeply concerning how casually people dismiss legitimate medical concerns in favor of fiscal convenience.
There is no ethical justification for replacing a prescribed medication with a generic substitute without explicit, documented consent.
The FDA’s ‘bioequivalence’ standard is not a guarantee of clinical parity.
Patients deserve the right to choose the formulation their physician originally prescribed - not the one that maximizes corporate profit.
This is not progress. It is coercion disguised as savings.
Elliot Barrett
Look I get it - generics save money
But honestly? I don’t care
I’d rather pay $300 and not wonder if my heart med is gonna fail
It’s not about the science - it’s about peace of mind
And if you’re the type who switches meds like trading cards, good for you
But don’t act like everyone else is dumb for wanting the brand
Katherine Chan
Y’all are overthinking this so hard
My mom’s been on generic warfarin for 12 years
She’s hiking in the Rockies at 78
She didn’t even know the difference until I told her she was saving $280 a month
And now she’s got a whole new wardrobe
Generics aren’t magic - they’re just smart
And if you’re scared, ask your pharmacist - they’ll hold your hand
But please stop making this a drama
It’s medicine, not a Netflix thriller 🙃
Tim Tinh
Just had my first generic switch last month - fexofenadine for my allergies
Thought I’d be sneezing all day but nope - same as before
Pharmacist was super chill and even showed me the FDA page
Turns out my brand name was made in the same factory as the generic
Went from $30 to $8 - that’s a coffee and a donut saved every month
Don’t overthink it - your body doesn’t care what the label says
Just make sure you’re not allergic to the dye - but that’s rare
And if you’re still worried? Talk to your doc - they’ll get it
Seriously - you’re not being reckless
You’re being smart 💪
Iris Carmen
my pill changed color and i thought i was gonna die
turns out it was just generic
now i save $200 a month
and i still dont know what the dye is but i’m alive so 🤷♀️
Ruth Witte
Generics = 💰💸🤑
My diabetes meds used to cost my whole paycheck
Now I can afford gas AND a treat
And my A1C is better than ever
Don’t let fear cost you your life
Ask for the generic - your future self will hug you 🤗❤️
Lauren Dare
The term ‘bioequivalence’ is a regulatory euphemism masking the commodification of physiological outcomes.
When you equate therapeutic equivalence with pharmacokinetic parameters, you reduce human biology to a controlled variable.
And yet - the FDA’s Orange Book is treated as gospel.
One must ask: who authored the standards? Who funded the trials?
And why are the most vulnerable populations being incentivized to trade uncertainty for affordability?
It’s not science. It’s systemic optimization.
And I’m not convinced it’s ethical.
Taya Rtichsheva
my pharmacist gave me the generic and i cried
not because i was scared
because i realized i’d been paying $250 for a pill that cost $4
and no one told me
so i told my mom
and now she’s switching too
we’re both gonna buy a vacation with the savings
and honestly
the pill still works
weird right?