Understanding Endometrial Hyperplasia
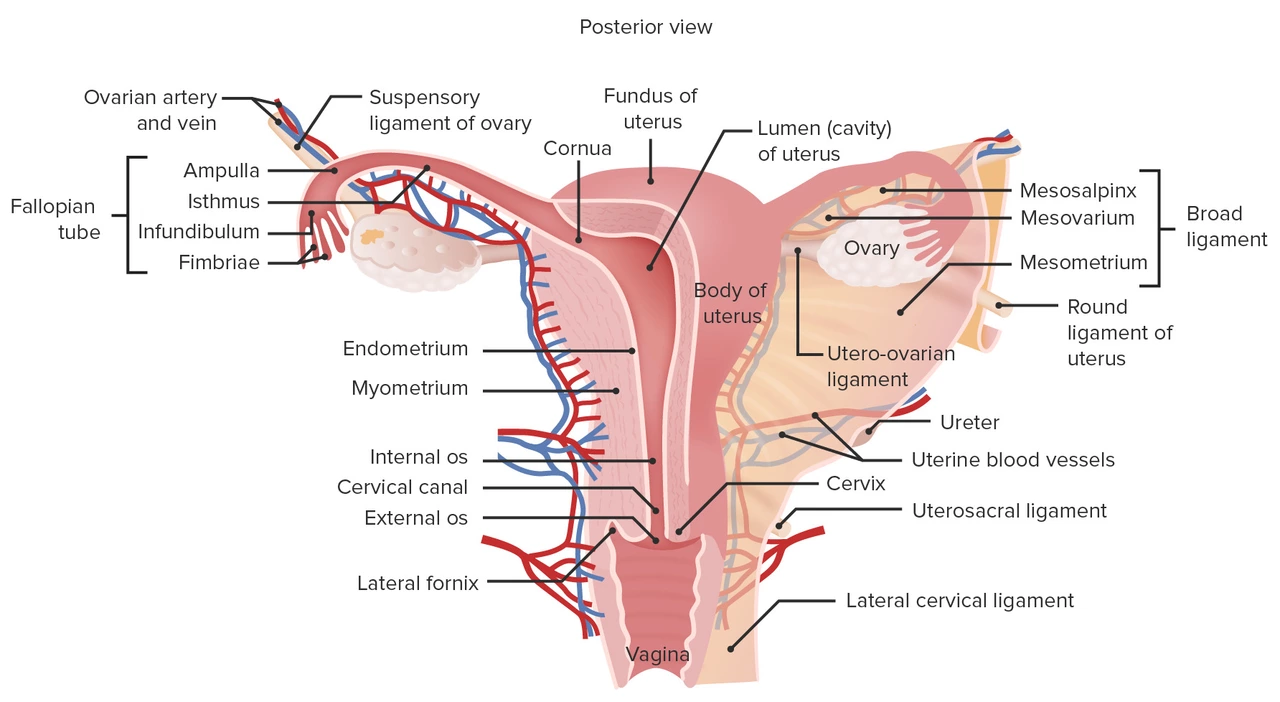
Before we dive into the role of endometrial hyperplasia in overgrowth of the uterine lining, it's essential to have a clear understanding of what endometrial hyperplasia is. Endometrial hyperplasia is a condition in which the uterine lining, also known as the endometrium, becomes thicker than usual. This thickening occurs due to an abnormal increase in the number of cells in the endometrium. The primary cause of endometrial hyperplasia is an imbalance of the hormones estrogen and progesterone, which regulate the growth and shedding of the uterine lining.
There are different types of endometrial hyperplasia, ranging from simple hyperplasia without atypia, which has a low risk of progressing to cancer, to complex hyperplasia with atypia, which has a higher risk of developing into endometrial cancer. Understanding the role of endometrial hyperplasia in the overgrowth of the uterine lining can help in diagnosing and treating this condition and preventing its possible complications.
The Connection Between Hormones and Endometrial Hyperplasia
Estrogen and progesterone play a crucial role in the normal functioning of the female reproductive system. Estrogen is responsible for the growth of the endometrium during the menstrual cycle, while progesterone ensures that this growth is regulated and the endometrium sheds properly during menstruation. When there is an imbalance between these two hormones, the endometrium may not shed as it should, leading to an overgrowth of the uterine lining.
Endometrial hyperplasia typically occurs when there is an excess of estrogen without the counterbalancing effect of progesterone. This can happen for various reasons, including obesity, polycystic ovary syndrome (PCOS), and the use of certain medications such as estrogen-only hormone therapy. Understanding the hormonal connection behind endometrial hyperplasia is essential for identifying the underlying cause and determining the appropriate treatment plan.
Symptoms and Diagnosis of Endometrial Hyperplasia
Endometrial hyperplasia often comes with a set of symptoms that can help in its early detection and diagnosis. Some common symptoms include abnormal uterine bleeding, such as heavy or prolonged periods, bleeding between periods, or postmenopausal bleeding. It's important to note that not all women with endometrial hyperplasia will experience these symptoms, and some may not have any symptoms at all.
To diagnose endometrial hyperplasia, doctors usually perform a series of tests, including a pelvic exam, ultrasound, and endometrial biopsy. The biopsy involves taking a small sample of the uterine lining to examine under a microscope, which can confirm the presence of hyperplasia and determine its type. Early diagnosis and treatment are crucial to prevent complications and reduce the risk of progression to endometrial cancer.
Treatment Options for Endometrial Hyperplasia
Treatment for endometrial hyperplasia depends on the underlying cause, the severity of the condition, and the patient's individual needs. Some common treatment options include:
Hormone Therapy
Hormone therapy is often the first line of treatment for endometrial hyperplasia, particularly when it is caused by an imbalance of estrogen and progesterone. Progesterone therapy can help to counteract the effects of excess estrogen and regulate the growth and shedding of the uterine lining. This can be administered in various forms, including oral medication, intrauterine devices (IUDs), or injections.
Weight Loss and Lifestyle Changes
For women who are overweight or obese, losing weight can help to restore hormonal balance and reduce the risk of endometrial hyperplasia. Additionally, making certain lifestyle changes, such as adopting a healthy diet, exercising regularly, and managing stress, can also help to improve overall health and prevent the recurrence of endometrial hyperplasia.
Surgery
In some cases, surgery may be necessary to treat endometrial hyperplasia, particularly when hormone therapy is not effective or the patient has a high risk of developing endometrial cancer. The most common surgical procedure for endometrial hyperplasia is a hysterectomy, which involves the removal of the uterus.
Risk Factors and Prevention
Understanding the risk factors for endometrial hyperplasia can help in its prevention. Some common risk factors include obesity, PCOS, early menstruation, late menopause, never having given birth, and a family history of endometrial, ovarian, or colon cancer. While not all of these risk factors can be controlled, making healthy lifestyle choices, such as maintaining a healthy weight and exercising regularly, can help to reduce the risk of developing endometrial hyperplasia.
Monitoring and Follow-up Care
Once endometrial hyperplasia has been diagnosed and treated, it's essential to have regular follow-up care to monitor the condition and ensure that it does not recur or progress to endometrial cancer. This may involve regular pelvic exams, ultrasounds, and endometrial biopsies, as well as ongoing communication with your healthcare provider about any changes in your symptoms or overall health.
Conclusion
Endometrial hyperplasia is a condition that affects the uterine lining and can lead to an overgrowth of the endometrium. It is primarily caused by an imbalance of estrogen and progesterone and can have various symptoms, such as abnormal uterine bleeding. Early diagnosis and treatment, including hormone therapy, lifestyle changes, and surgery, are essential to prevent complications and reduce the risk of progression to endometrial cancer. Understanding the role of endometrial hyperplasia in the overgrowth of the uterine lining can help to promote awareness, early detection, and effective treatment of this condition.

Joe Murrey
Interesting read, thx!
Tracy Harris
The discussion of hormonal imbalance necessitates a comprehensive examination of endocrine pathways. Estrogen dominance, unmitigated by progesterone, constitutes a pivotal factor in endometrial hyperplasia. Moreover, the correlation between obesity and peripheral aromatization underscores a metabolic dimension that should not be overlooked. While the article aptly outlines therapeutic avenues, it omits a nuanced analysis of progestin delivery mechanisms. Consequently, clinicians may benefit from an expanded discourse on dosage optimization. An elevated standard of scholarly rigor is advocated.
Sorcha Knight
Whoa, this stuff is wild! 😮 The way estrogen can just take over the lining is like a drama series that never ends. I love how the article breaks down the risks, but also makes it sound so real‑life relatable. Definitely a must‑read for anyone dealing with weird bleedings.
Jackie Felipe
I think u should also look at diet and exercise. Weight loss can really help.
debashis chakravarty
The pathophysiology of endometrial hyperplasia is rooted in an unopposed estrogenic stimulus. In the absence of sufficient progesterone, the proliferative phase persists beyond its physiological limits. This persistent proliferation manifests histologically as an increased gland-to-stroma ratio. Epidemiological data reveal a striking association between obesity and heightened peripheral estrogen conversion. Polycystic ovary syndrome further exacerbates the endocrine milieu by augmenting androgen levels that aromatize to estrogen. Consequently, patients present with a spectrum of abnormal uterine bleeding patterns, ranging from menorrhagia to intermenstrual spotting. Diagnostic algorithms should prioritize transvaginal ultrasonography to assess endometrial thickness. A subsequent endometrial biopsy remains the gold standard for definitive histopathological classification. Histologic subtypes, including simple hyperplasia without atypia and complex hyperplasia with atypia, carry disparate oncologic prognoses. Therapeutic strategies must be individualized, with progestogenic agents constituting first‑line therapy for most presentations. The levonorgestrel‑releasing intrauterine system offers a localized high‑dose approach with favorable safety profiles. In refractory cases, particularly when atypia is present, hysterectomy may be indicated to mitigate malignant transformation. Lifestyle modification, notably weight reduction, serves as an adjunctive measure to restore hormonal equilibrium. Ongoing surveillance through periodic ultrasounds and, when indicated, repeat biopsies is essential to detect recurrence. Ultimately, a multidisciplinary approach integrating endocrinology, gynecology, and patient education optimizes outcomes and reduces the burden of disease.
Daniel Brake
One might contemplate the philosophical implications of hormonal balance as a metaphor for equilibrium in broader life contexts. It invites reflection on how excess and deficiency shape our experiences. Such analogies may foster deeper patient empathy.
Emily Stangel
In reviewing the presented material, one is struck by the comprehensive overview of both etiologic and therapeutic dimensions. The delineation between simple and complex hyperplasia provides a clear framework for risk stratification. Moreover, the emphasis on lifestyle interventions underscores the importance of patient‑centered care. While hormonal therapy remains paramount, the discussion of intrauterine devices adds valuable nuance. The surgical considerations are aptly contextualized, noting hysterectomy as a definitive option for refractory cases. Follow‑up protocols, including periodic imaging and biopsies, are well articulated, ensuring vigilance against recurrence. Overall, the synthesis of pathophysiology, clinical presentation, and management embodies an exemplary educational resource for both trainees and seasoned clinicians.
Suzi Dronzek
The preceding exposition, while thorough, could benefit from a more granular analysis of progestin dosing regimens. A comparative table illustrating oral, injectable, and intrauterine delivery would enhance clinical decision‑making. Additionally, the omission of emerging molecular markers limits the article’s forward‑looking relevance. Addressing these gaps would elevate the discourse to a truly evidence‑based pinnacle. The authors are encouraged to incorporate such refinements in subsequent revisions. Until then, readers must supplement the narrative with external resources.
Aakash Jadhav
Yo, that table would be fire! 🔥 Can't wait to see the side‑by‑side showdown.
Amanda Seech
Great summary! I think it really helps people understand why diet and exercise matter.
Elizabeth Nisbet
Exactly! Keep focusing on those lifestyle tweaks and you’ll see big improvements.
Sydney Tammarine
Whoa, the drama of hormones is like a soap opera you can’t stop watching! 😂 The way estrogen just storms the stage, and progesterone tries to calm it down-total chaos, love it!
Shawn Simms
The metaphorical description is vivid, yet clinical precision remains essential. Accurate terminology ensures that readers can translate this narrative into practice without ambiguity. Maintaining a balance between engaging prose and scientific rigor is advisable.
Drew Chislett
All in all, this is a solid guide-keep the optimism flowing and remember every small step counts toward better health.
Rosalee Lance
Honestly, I think the mainstream medical community is hiding the truth about hormonal hacks. They don’t want us to know about natural ways to rebalance estrogen-big pharma’s agenda, right? Stay woke and keep questioning what they feed you.
Kara Lippa
Thanks for the thorough walkthrough-your calm tone makes a complex topic feel approachable.
Avinash Sinha
Yo, that calm vibe is cool, but let’s splash some color on this! Imagine the uterus as a canvas and hormones as wild paint-sometimes it’s a masterpiece, sometimes a mess!
Avinash Sinha
Exactly! And when the paint spills, you gotta grab a bigger brush-aka a stronger progestin-and clean up the chaos.