Pharmacist Safety: Protecting Yourself and Patients from Medication Errors
When we talk about pharmacist safety, the practices and systems that ensure pharmacists can dispense medications accurately without putting themselves or patients at risk. It's not just about counting pills—it's about catching deadly mistakes before they happen. A single misread prescription, a mix-up between similarly named drugs, or an unchecked interaction can turn a routine visit into a life-threatening event. In fact, studies show that over 1.5 million preventable adverse drug events happen each year in the U.S. alone, and pharmacists are often the last line of defense.
medication errors, mistakes in prescribing, dispensing, or taking drugs that can lead to harm don’t always come from carelessness. They’re often hidden in busy workflows, poor handwriting, confusing brand names, or overlapping drug classes. For example, mixing warfarin and antibiotics, a dangerous combination that can spike bleeding risk—as seen in post 69361—is a classic case where pharmacist vigilance saves lives. Same goes for acid-reducing medications, like PPIs that block absorption of critical drugs such as HIV and cancer treatments (post 71607). These aren’t hypothetical risks. They’re daily realities in pharmacies worldwide.
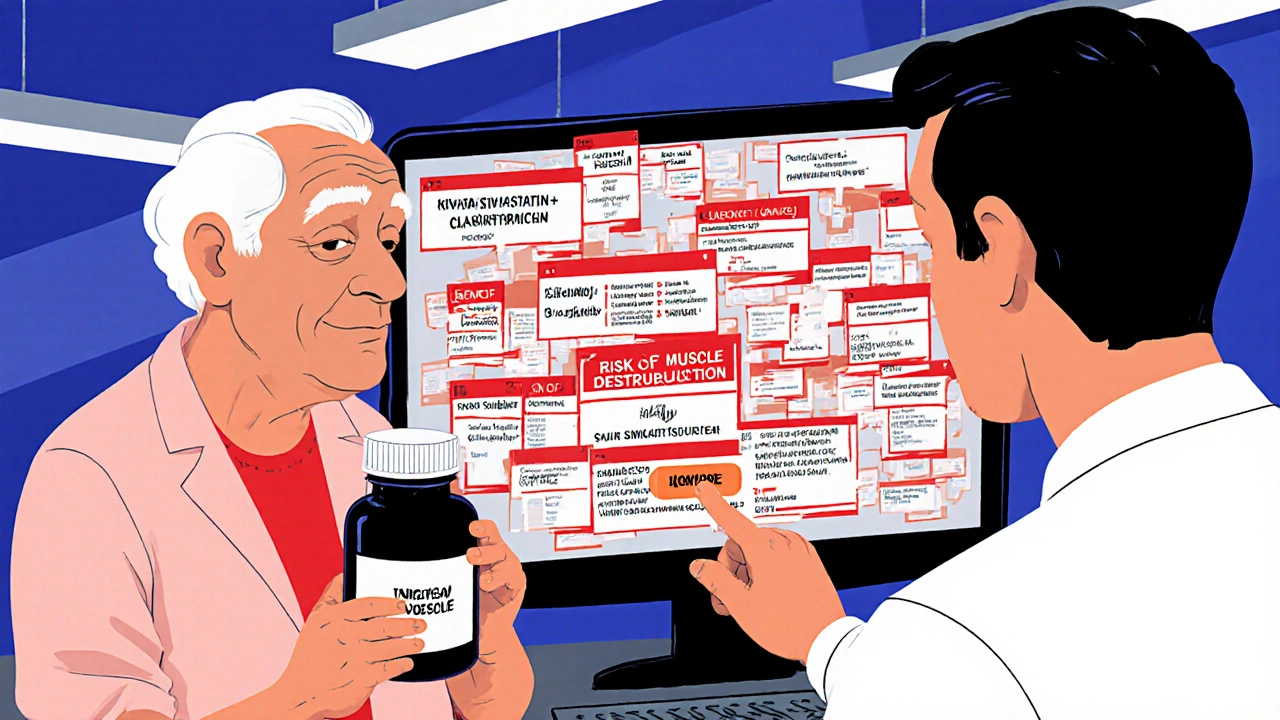
drug interactions, when two or more medications affect each other’s effectiveness or safety are everywhere. One wrong combination can turn a safe treatment into a crisis. That’s why pharmacist safety includes double-checking every script against a patient’s full list—especially when they’re on multiple drugs like dual antiplatelet therapy, which combines aspirin and clopidogrel to prevent clots but raises bleeding risk (post 71120). Even something as simple as first-generation antihistamines, like Benadryl, which can cause confusion and memory loss in older adults (post 64945), needs scrutiny. Pharmacists don’t just fill orders—they interpret them.
And it’s not just about what’s in the bottle. pharmacy errors, mistakes caused by system flaws, staffing shortages, or poor labeling are just as dangerous. A mislabeled generic, a misprinted dosage, or a rushed refill can all lead to harm. That’s why reporting rare side effects from generics—like in post 69822—isn’t just a formality. It’s part of the safety chain. Every time a pharmacist speaks up, they help fix broken systems.
Real pharmacist safety means having the time, tools, and training to spot these risks. It means knowing when to pause, ask, and verify—even when the line is long. It means understanding that a statin causing muscle pain (post 75711) or an antibiotic messing with warfarin (post 69361) isn’t just a side effect—it’s a warning sign that needs action. And it means recognizing that patients often don’t know what to ask. That’s where the pharmacist steps in.
Below, you’ll find real-world examples of how medication risks show up—and how pharmacists, doctors, and patients can work together to stop them before they hurt someone.
Red Flags in Drug Interactions: Combinations Your Pharmacist Should Question
- Nov, 18 2025
- Daniel Remedios
- 9 Comments
Certain drug combinations can be deadly - yet many pharmacies miss them. Learn the top five dangerous interactions pharmacists must catch, why they’re often overlooked, and what you can do to protect yourself.
