Gastric Acid Hypersecretion: Understanding Causes, Risks, and Management
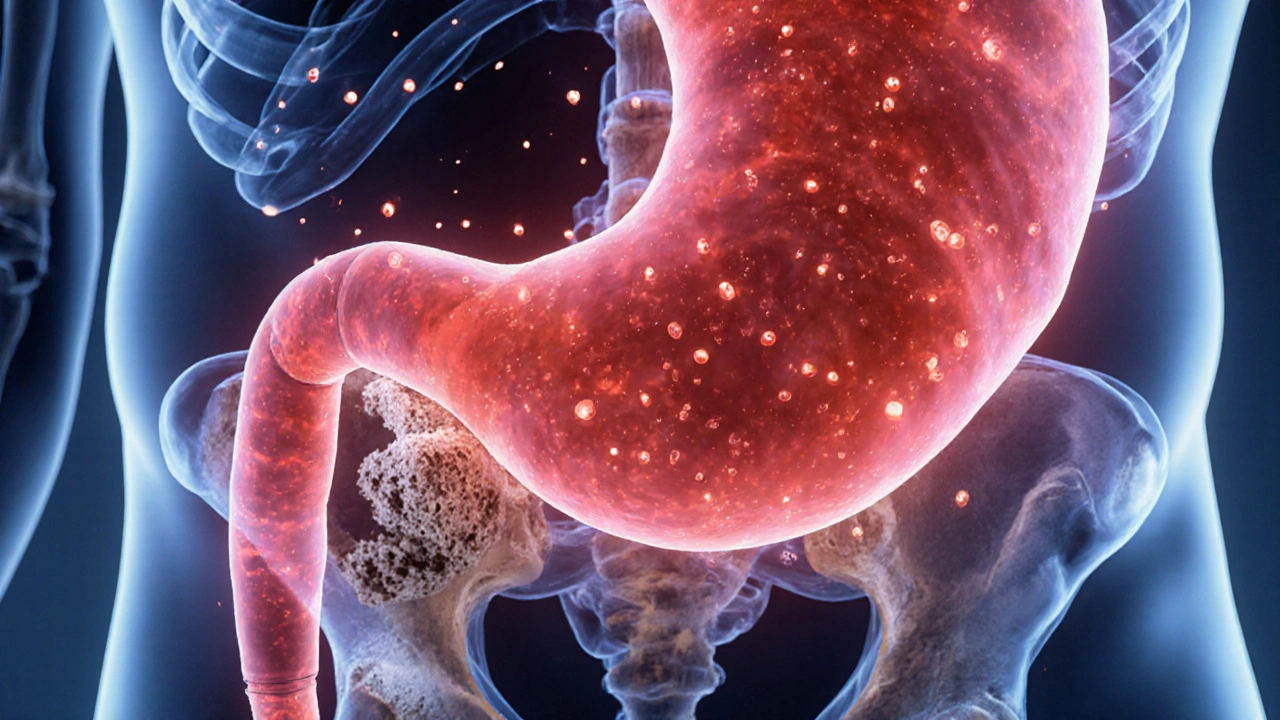
When dealing with gastric acid hypersecretion, excess production of stomach acid that can erode the mucosa and trigger pain, reflux, or ulceration, the first thing to know is that it’s not just a stomach‑issue. It often sets off a chain reaction: the extra acid can push up into the esophagus, leading to GERD, gastro‑esophageal reflux disease, a condition where stomach acid repeatedly flows back into the esophagus. In turn, that reflux can wear down the lining of the stomach or duodenum, paving the way for peptic ulcer disease, sores that develop on the stomach or duodenal lining due to acid damage. The basic semantic chain looks like this: gastric acid hypersecretion → GERD → increased ulcer risk. Understanding that chain helps you pick the right treatment and lifestyle tweaks early on.
One of the most common ways doctors break the chain is with a proton pump inhibitor, a class of drugs that block the final step of acid production in stomach cells. These meds lower the overall acid load, which reduces the chance of reflux and gives ulcer tissue a chance to heal. They’re often paired with diet changes, because cutting back on caffeine, alcohol, and spicy foods cuts the “fuel” that drives the hyper‑secretion. If you’ve tried over‑the‑counter antacids and still feel that burning sensation, a prescription‑strength proton pump inhibitor may be the next logical step.
Beyond meds, it’s worth knowing there are other conditions that can masquerade as simple acid over‑production. Zollinger‑Ellison syndrome, for example, is a rare tumor that cranks up gastrin levels, which in turn super‑charges acid output. While it’s not common, spotting the extra‑ordinary signs—like ulcers that don’t heal or acid reflux that’s resistant to standard therapy—can prompt a deeper work‑up. In most cases, though, lifestyle factors play a bigger role. Smoking, late‑night meals, and high‑fat diets all stimulate the stomach’s acid‑producing cells, making the whole system more volatile.
Speaking of lifestyle, the day‑to‑day habits you choose can either calm or aggravate the problem. Eating smaller meals more frequently keeps the stomach from becoming overly full, which reduces pressure that forces acid upward. Staying upright for at least two hours after eating gives gravity a hand in keeping the acid where it belongs. Even simple moves like raising the head of your bed by a few inches can cut nighttime reflux dramatically. The goal is to create an environment where the stomach doesn’t feel the need to over‑produce acid to digest a massive, high‑fat feast.
When you suspect gastric acid hypersecretion, a doctor will usually start with a few key tests. An upper endoscopy lets the specialist peek directly at the lining and spot any existing ulcers. A pH monitoring study measures how often acid reaches the esophagus over a 24‑hour period, giving a clear picture of reflux severity. Blood tests for gastrin can uncover hidden tumors like Zollinger‑Ellison. Armed with these data points, the clinician can tailor a plan that mixes medication, diet tweaks, and, when needed, surgery.
All of this background sets the stage for the range of articles you’ll see below. From detailed drug comparisons to lifestyle guides and disease overviews, the collection offers practical steps you can take whether you’re dealing with occasional heartburn or a chronic acid‑related condition. Dive in to find the specific advice that fits your situation and start taking control of your stomach health today.
Zollinger-Ellison Syndrome and Osteoporosis Risk: What You Need to Know
- Oct, 12 2025
- Daniel Remedios
- 16 Comments
Learn how Zollinger-Ellison syndrome raises osteoporosis risk, how to spot early bone loss, and practical steps to protect your skeleton while managing acid issues.
