Dangerous Medication Combinations: What You Must Avoid to Stay Safe
When you take more than one medicine, you’re not just adding effects—you’re creating new risks. dangerous medication combinations, mixes of drugs that can cause serious harm by changing how each one works in your body. These aren’t rare mistakes—they happen every day, often because people don’t realize their pills can clash. A common example? Warfarin, a blood thinner, and certain antibiotics. Together, they can spike your bleeding risk or make the blood thinner useless. That’s not a theory—it’s why doctors check your INR levels when you start a new antibiotic. Same goes for acid-reducing drugs like PPIs. They’re meant to calm heartburn, but they also block your body from absorbing critical drugs like HIV meds, antifungals, and even some cancer treatments. Your stomach acid isn’t just for digestion—it’s a gatekeeper for medicine absorption.
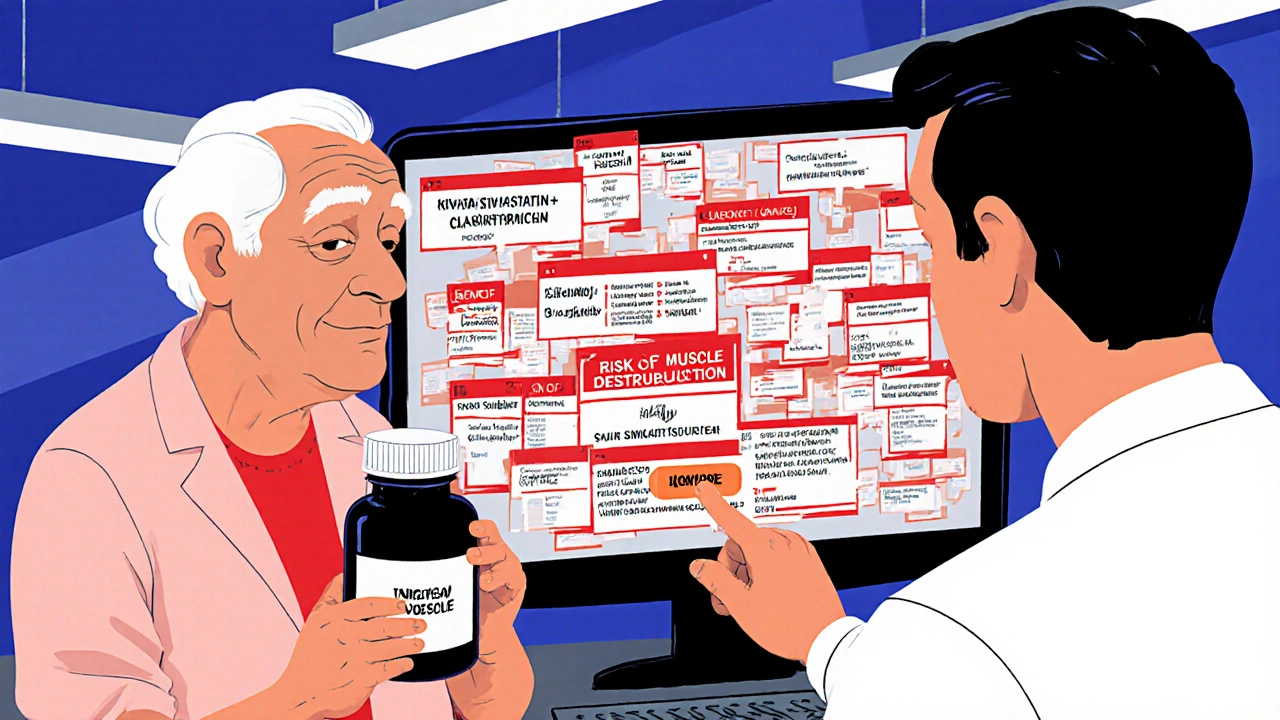
Then there’s the quiet danger: statins. These cholesterol-lowering pills help millions avoid heart attacks, but when paired with certain antibiotics or grapefruit juice, they can turn muscle pain into a life-threatening condition called rhabdomyolysis. It’s not just about one bad combo—it’s about stacking risks. Antipsychotics for psychosis? Fine, unless you have Parkinson’s. Then they can freeze your movement, making tremors and stiffness worse. That’s because they block dopamine, the very chemical Parkinson’s patients are already low on. And it’s not just old drugs. Even something as simple as first-generation antihistamines like Benadryl can build up over time and raise your dementia risk, especially if you’re on other meds that affect your brain. These aren’t isolated issues—they’re part of a pattern where common prescriptions interact in ways most patients never hear about until something goes wrong.
You don’t need to memorize every possible clash. But you do need to know the big ones: blood thinners, heart meds, antibiotics, acid reducers, and pain relievers. These are the usual suspects. If you take more than three pills a day, you’re in the high-risk zone. And if you’re over 65, or have liver or kidney trouble, your body doesn’t clear drugs the same way. That’s why your pharmacist isn’t just handing out bottles—they’re your last line of defense. The posts below dig into real cases: how warfarin and antibiotics can turn a simple infection into a hospital trip, why statins and certain foods are a bad mix, how acid blockers sabotage cancer treatment, and why some painkillers slow healing instead of helping. These aren’t theoretical warnings. These are stories from real people who learned the hard way. What you’re about to read could keep you out of the ER.
Red Flags in Drug Interactions: Combinations Your Pharmacist Should Question
- Nov, 18 2025
- Daniel Remedios
- 9 Comments
Certain drug combinations can be deadly - yet many pharmacies miss them. Learn the top five dangerous interactions pharmacists must catch, why they’re often overlooked, and what you can do to protect yourself.
