Cholesterol Lowering: What Works, What Doesn’t, and What Your Doctor Isn’t Telling You
When it comes to cholesterol lowering, the process of reducing harmful blood fats to prevent heart disease. Also known as lipid management, it’s not just about popping a pill—it’s about understanding what’s actually moving the needle on your numbers. Most people think statins are the only answer, but that’s not the whole story. High LDL cholesterol isn’t a disease by itself—it’s a warning sign. And how you respond to it makes all the difference.
Real cholesterol lowering isn’t just about drugs. It’s about how your body handles LDL cholesterol, the main type of bad cholesterol that builds up in artery walls. Some people see big drops on a low-fat diet. Others barely move—until they cut out refined carbs and sugar. That’s because triglycerides and HDL don’t respond the same way to every change. Your liver makes most of your cholesterol, and what you eat can either calm it down or rev it up. Statins, a class of drugs that block cholesterol production in the liver work well for many, but they’re not magic. They can cause muscle pain, raise blood sugar, and don’t fix the root cause if your diet is still full of processed foods. And here’s the thing: if your triglycerides are high and HDL is low, no statin will fix that alone. You need lifestyle changes—real ones, not just "eat less fat."
Diet for cholesterol, the pattern of food choices that directly impact blood lipid levels is the most powerful tool most people ignore. Soluble fiber from oats, beans, and apples pulls cholesterol out of your system. Omega-3s from fatty fish lower triglycerides. Plant sterols in fortified foods block cholesterol absorption. And trans fats? They’re worse than saturated fat—still lurking in packaged snacks and fried foods. But here’s what no one tells you: cutting out bread and sugar often lowers LDL more than cutting out butter. Your body turns excess sugar into fat, and that fat ends up in your bloodstream.
Cholesterol lowering isn’t one-size-fits-all. Someone with familial hypercholesterolemia needs strong meds. Someone with metabolic syndrome needs a different plan. And if you’re on a statin but still have high triglycerides, you’re not done. That’s when your doctor should consider fibrates or omega-3s. But too many doctors skip the basics and just prescribe. You need to know what your numbers mean—not just that they’re "high."
What you’ll find in the articles below isn’t fluff or hype. It’s real, practical info on how drugs like statins interact with other meds, what supplements actually help (and which ones are waste), and how everyday choices—like sleep, stress, and even antibiotics—can quietly mess with your lipid levels. No theory. No jargon. Just what works, what doesn’t, and why.
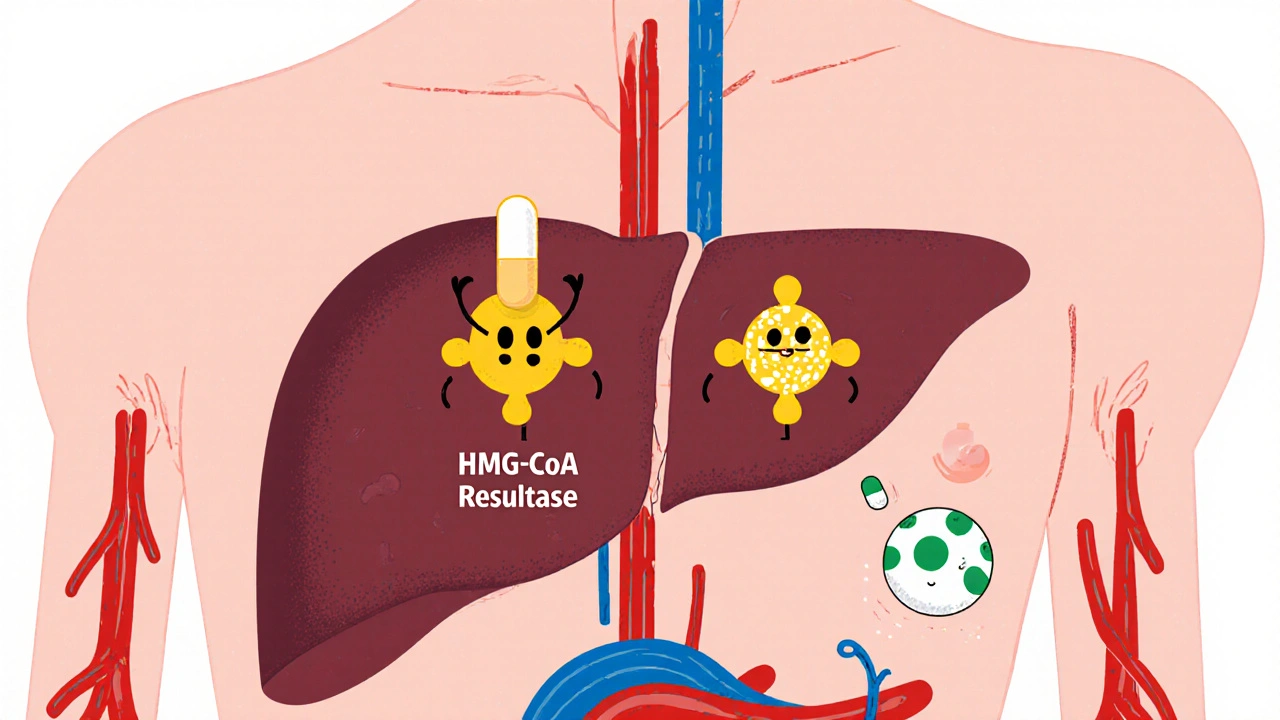
Statin Medications: How They Lower Cholesterol and What You Need to Know About Muscle Pain
- Nov, 20 2025
- Daniel Remedios
- 12 Comments
Statins lower cholesterol and cut heart attack risk by up to 30%, but muscle pain affects up to 29% of users. Learn how they work, which statins cause fewer side effects, and what to do if you experience muscle pain.
