When you pick up a prescription at your local pharmacy, you might not think twice if the pill looks different from last time. That’s generic substitution in action. But if you’re admitted to the hospital and your IV antibiotic gets swapped out for a different brand, that’s something else entirely. The way medications are substituted in retail versus hospital pharmacies isn’t just a technical difference-it’s a fundamental shift in how care is delivered, who makes the call, and why.
Who Decides? Retail vs Hospital Substitution Authority
In a retail pharmacy, the pharmacist has the legal right to swap a brand-name drug for a generic version, as long as the state allows it and the prescriber hasn’t blocked it. This isn’t a suggestion-it’s part of the job. Every state in the U.S. permits this under their pharmacy practice laws. The pharmacist checks the prescription, sees the insurance will pay less for the generic, and hands you the cheaper version. You might get a notice, maybe a quick chat, but the decision is mostly automated by formulary rules and cost-saving targets. In a hospital, no single pharmacist makes that call alone. Substitutions here happen through Pharmacy and Therapeutics (P&T) committees. These are teams of doctors, pharmacists, nurses, and administrators who review clinical data, cost impact, and safety outcomes before approving a drug swap. If a hospital wants to switch from one beta-lactam antibiotic to another to cut costs or reduce resistance, the P&T committee votes on it. Then, protocols are written, staff are trained, and the change rolls out across units. It’s not a point-of-sale decision-it’s a clinical strategy.What Gets Substituted? Types of Medications
Retail substitution is mostly about pills and capsules. Over 97% of substitutions in community pharmacies involve oral solid dosage forms-think blood pressure meds, cholesterol drugs, or antibiotics like amoxicillin. These are easy to swap because they’re stable, well-studied, and have clear bioequivalence data. Hospitals deal with far more complex drugs. Nearly 70% of therapeutic interchanges involve intravenous medications, biologics, or compounded formulations. For example, switching from brand-name vancomycin to a generic version isn’t just about price-it’s about ensuring the IV concentration, infusion rate, and stability match clinical needs. Biologics like insulin or monoclonal antibodies are trickier still. While generics (called biosimilars) exist, hospitals have stricter protocols before switching them, often requiring physician approval and patient monitoring.Why Do They Swap? Different Goals
Retail substitution is driven by money. Insurance companies push for generics because they save billions. In 2023, generic drugs saved the U.S. healthcare system $317 billion-most of it from retail pharmacies. Pharmacists report that 92% of their substitution decisions are influenced by insurance formularies. If the patient’s plan won’t cover the brand, the generic is the only option unless the doctor fights it. Hospital substitution is driven by clinical outcomes. Hospital pharmacists aren’t just saving money-they’re improving safety and effectiveness. A 2022 survey found that 85% of hospital pharmacists say patient-specific factors like kidney function, drug interactions, or infection type guide their substitution choices. For instance, swapping from a broad-spectrum antibiotic to a targeted one can reduce C. difficile infections by up to 30% in some units. It’s not about cost alone-it’s about better care.
How Are Patients Told? Notification Rules
In retail, patients have rights. Forty-seven states require pharmacists to notify patients when a substitution is made. Some states require verbal notice, others require written consent-especially for the first substitution. Many pharmacists hand out printed sheets explaining the change. This is partly because patients often confuse generics with lower quality. One Consumer Reports survey found 14% of patients thought a generic was "weaker" or "less effective." Pharmacists spend time reassuring them. In hospitals, patients rarely get direct notice. The substitution happens behind the scenes. The doctor is notified within 24 hours, and the change is logged in the electronic health record. The patient might never know their antibiotic was switched unless they ask. This isn’t secrecy-it’s efficiency. In a busy ICU, interrupting care for a substitution explanation isn’t practical. Instead, the medical team is trained on the new protocol, and the change is embedded in the workflow.Documentation: Paper Trail vs Digital Integration
Retail pharmacies keep substitution records for two years, usually in their dispensing software. These records are for compliance, not clinical use. They’re rarely reviewed unless there’s a complaint or audit. Hospitals integrate substitution data into the EHR. Every swap triggers an alert in the system. The change appears in the patient’s medication list, flows to nursing charts, and can be flagged during discharge planning. This is required by CMS regulations to prevent errors during transitions of care. If a patient leaves the hospital on a new drug, the pharmacy must ensure the outpatient pharmacy knows about it-otherwise, the patient might get the wrong one at the retail counter.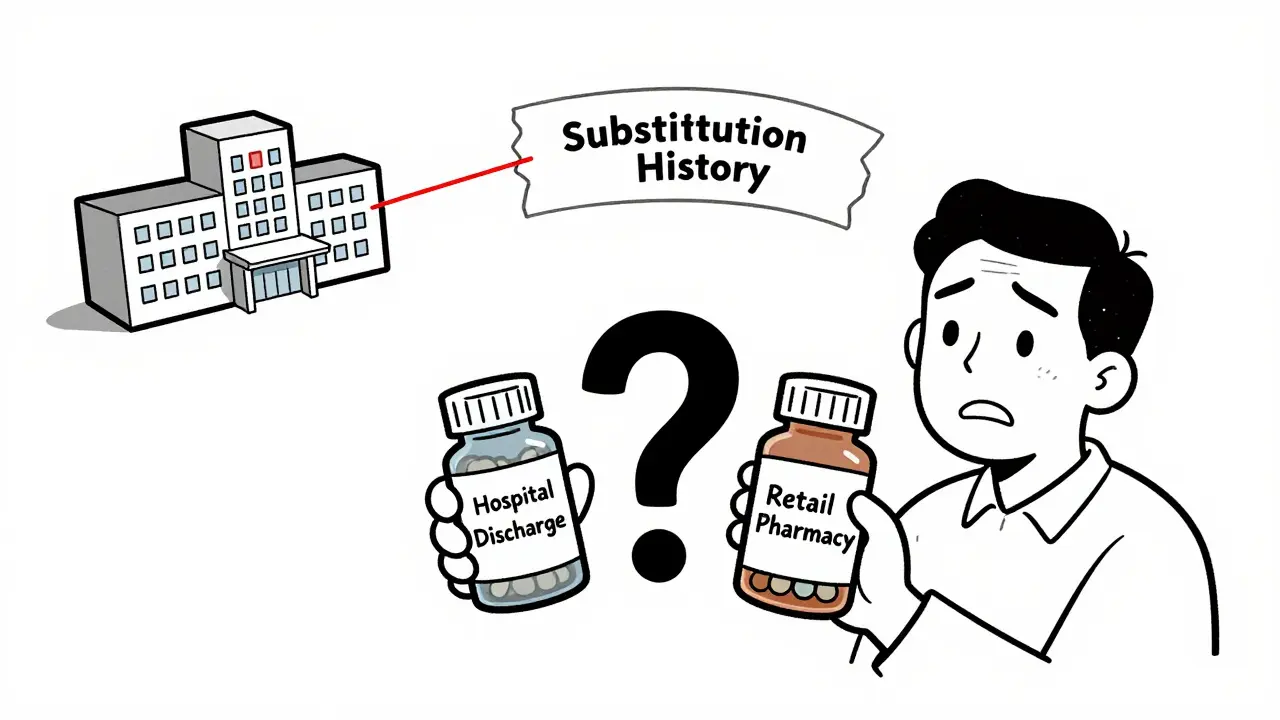
Challenges and Risks
Retail pharmacists face daily friction with insurance companies. Over 60% report delays from prior authorizations, forcing them to call insurers multiple times just to get a generic approved. Patients get frustrated. Pharmacists feel caught in the middle. Hospital pharmacists battle physician resistance. Even when a P&T committee approves a substitution, some doctors refuse to adopt it. One study found 57% of hospital pharmacists say clinician buy-in is their biggest hurdle. Changing long-standing prescribing habits takes education, data, and persistence. But the biggest risk? The gap between hospital and retail. When a patient is discharged, their hospital medication might be swapped to a different generic than what they used before. A 2022 ISMP report found that nearly 24% of medication errors during hospital-to-home transitions involve substitution mismatches. A patient might come home on a generic lisinopril, but their old bottle had a different manufacturer. If the pharmacist doesn’t catch it, the patient could get confused, miss a dose, or even have a reaction.Where Is This All Headed?
The system is slowly starting to connect. New federal rules, like the 2024 CMS Interoperability Rule, require pharmacies and hospitals to share substitution history electronically. Companies like Epic and Cerner are building tools that will show a patient’s entire substitution history-whether it happened in the hospital or at CVS. Some hospitals now have discharge pharmacists who call the patient’s retail pharmacy to align medications. Retail chains are starting to ask for hospital discharge summaries when patients bring in new prescriptions. These are small steps, but they matter. The future isn’t about choosing one model over the other. It’s about coordination. Retail pharmacies will keep saving money through generics. Hospitals will keep optimizing care through clinical swaps. But if they don’t talk to each other, patients pay the price.Can a retail pharmacist refuse to substitute a medication?
Yes, but only under specific conditions. A retail pharmacist can refuse substitution if the prescriber writes "Do Not Substitute" on the prescription, if the patient declines it, or if state law prohibits substitution for that drug (like certain controlled substances). Pharmacists can also refuse if they believe the generic is inappropriate for the patient’s condition, though this is rare and requires documentation.
Are hospital substitutions always cheaper than retail ones?
Not always. While hospital substitutions often aim to reduce costs, their primary goal is clinical improvement. Sometimes a hospital will switch to a more expensive drug if it reduces complications or hospital stays. For example, switching from a generic antibiotic to a newer one that lowers infection rates might cost more upfront but save money overall by preventing longer hospitalizations.
Why can’t I get the same generic at the hospital that I use at home?
Hospitals use formularies based on bulk purchasing, stability, and compatibility with their systems. The generic your retail pharmacy dispenses might not be available in the hospital’s supply chain, or it might not meet the hospital’s quality standards for IV use. Even if two generics are chemically identical, the fillers, coating, or manufacturing process can affect how they behave in a clinical setting.
Do biosimilars follow the same substitution rules in retail and hospital settings?
No. Biosimilars are more complex than traditional generics. In retail, 23 states have laws allowing pharmacists to substitute biosimilars without physician approval-but only if the FDA has designated them as "interchangeable." In hospitals, substitution of biosimilars almost always requires P&T committee approval and physician notification, regardless of FDA designation, due to higher risk and monitoring needs.
What should I do if I notice a medication change after being discharged from the hospital?
Always ask your pharmacist or doctor. Bring your hospital discharge summary and the new prescription with you. Ask: "Was this change intentional? Is it the same drug, just a different brand?" If you’re unsure, don’t take it. Many medication errors happen because patients assume the change is safe. Pharmacists are trained to catch these mismatches-use them as your safety net.


Joe Bartlett
Generics are just as good, honestly. If your blood pressure med looks different, you’re not getting ripped off. UK’s NHS does this daily and folks are fine.
Naomi Lopez
It’s fascinating how retail pharmacies have turned substitution into a cost-driven transaction, while hospitals treat it as a clinical decision. The former is commodified healthcare; the latter, ideally, is evidence-based medicine. One’s a vending machine, the other’s a symphony.
Salome Perez
As someone who’s worked in both settings, I’ve seen how chaotic the disconnect can be. I once had a patient come in with three different generics for the same drug-hospital discharge, home pharmacy, and a refill from a different CVS. She was terrified she was taking poison. We spent an hour mapping it all out. It’s not just about pills-it’s about trust.
Hospitals have protocols, but retail? Sometimes it’s a lottery. The system needs to talk to itself. We’re not just saving money-we’re saving lives from confusion.
Evelyn Vélez Mejía
There’s an unspoken hierarchy in pharmaceutical substitution: the retail pharmacist is a gatekeeper of cost; the hospital pharmacist is a guardian of clinical integrity. But when these worlds collide-when a patient leaves the hospital and walks into a pharmacy with no context-it’s not a system failure. It’s a moral one.
We’ve reduced medicine to algorithms and formularies, forgetting that the patient is not a data point, but a person who wakes up every morning wondering if the pill in their hand is the same one that kept them alive yesterday. That’s the real crisis-not the cost, but the erasure of continuity.
Victoria Rogers
lol so the hospital is "clinical" but they swap meds without telling you? sounds like a corporate cover-up. i bet they’re doing it to push fake biosimilars made in china. also, why do you trust a "committee"? they’re all pharma shills.
Pawan Chaudhary
Great breakdown! I work in pharmacy in India and we face similar issues-cost vs. care. But here, patients often don’t even know what a generic is. Education matters as much as policy. Keep sharing stuff like this!
Jonathan Morris
Let’s be real-this whole "P&T committee" is just Big Pharma’s backdoor. They fund the studies, the doctors get kickbacks, and suddenly your $300 drug is now a "clinical upgrade." The real substitution? Your trust in the system. They’re not saving you money-they’re locking you into their ecosystem.
BETH VON KAUFFMANN
Formulary-driven substitution in retail is a regulatory arbitrage play. The P&T committee model in hospitals represents institutionalized clinical governance-but it’s still subject to institutional capture. The real issue? Lack of interoperability between EHRs and pharmacy dispensing systems. We’re not talking about pharmacology-we’re talking about data silos masquerading as healthcare.
Jessica Salgado
I had a friend who went from hospital to home and got a different generic for her thyroid med. She felt like a zombie for three weeks. No one told her. No one asked. She almost didn’t make it to her follow-up. I cried reading this. It’s not just a pill. It’s your body remembering what it’s used to. Why do we treat medicine like a Walmart product?
Chris Van Horn
Let’s not pretend hospitals are saints. The "clinical strategy" you romanticize? It’s often just a thinly veiled cost-cutting exercise disguised as "evidence-based." And don’t get me started on biosimilars-those are just branded generics with a fancy name and a $50,000 marketing budget. You think patients don’t notice the difference? They feel it. They just don’t have the vocabulary to call it out.
And the "interoperability" you’re so proud of? It’s a scam. Epic and Cerner are profit-driven monopolies. They don’t want your data to flow-they want you locked into their ecosystem. This isn’t progress. It’s corporate consolidation with a white coat.