Relative Infant Dose Calculator
Estimate Baby's Medication Exposure
Enter details below to calculate the relative infant dose (RID) for common antidepressants during breastfeeding.
Results
When a new mom feels overwhelming sadness, exhaustion, or numbness after having a baby, it’s not just the sleep deprivation talking. Postpartum depression (PPD) affects about 1 in 8 women within the first year after childbirth. It doesn’t go away on its own. Left untreated, it can interfere with bonding, feeding, and even the baby’s development. But here’s the real dilemma: if you’re breastfeeding, which antidepressants are safe? And what side effects might your baby actually experience?
Why Untreated Depression Is Riskier Than Medication
Many mothers hesitate to take antidepressants while breastfeeding because they fear harming their baby. But the truth is, the risks of untreated depression are far greater. The American College of Obstetricians and Gynecologists (ACOG), the CDC, and the American Academy of Pediatrics all agree: a mother who is depressed, withdrawn, or unable to care for her baby puts the infant at higher risk than even the most commonly prescribed antidepressants.Depression can lead to poor feeding, missed well-baby visits, and even neglect. Babies of mothers with untreated PPD are more likely to have delayed language development, sleep problems, and emotional regulation issues later on. Meanwhile, the amount of medication that passes into breast milk is tiny-often less than 1% of the mother’s dose. That’s why experts say: treating the mother is treating the baby.
Which Antidepressants Are Safest for Breastfeeding?
Not all antidepressants are created equal when it comes to breastfeeding. The key metric doctors use is the relative infant dose (RID)-how much of the drug the baby actually gets through milk, adjusted for their weight. Anything under 10% RID is generally considered safe.Here’s the real-world ranking based on decades of data:
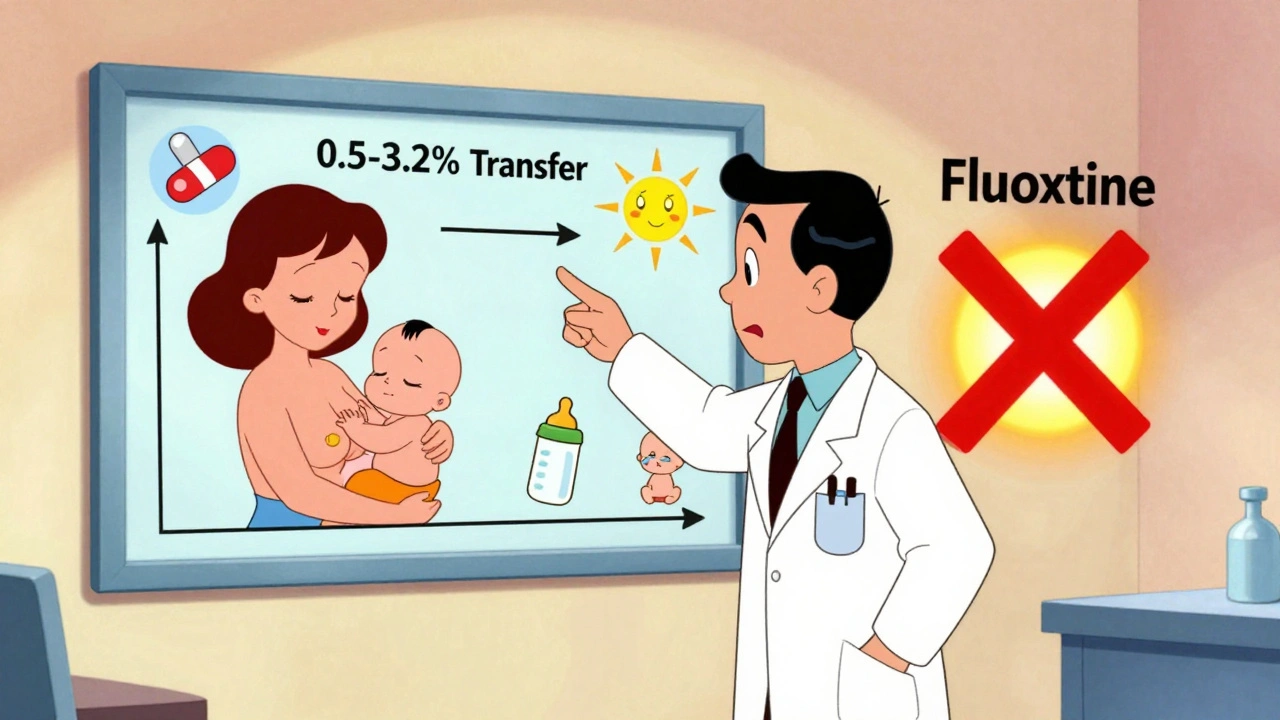
- Sertraline (Zoloft): The gold standard. Only 0.5-3.2% of the mom’s dose ends up in breast milk. In over 1,800 mother-baby pairs studied, 92% of infants had undetectable levels. Most moms report no changes in their babies’ sleep, feeding, or mood.
- Paroxetine (Paxil): Slightly higher transfer than sertraline (0.9-8.6%), but still low. Has the least amount of buildup in the baby’s system. Often preferred if mom has anxiety along with depression.
- Citalopram (Celexa): Moderate transfer (3.5-8.9%). Generally safe, but avoid doses above 40mg daily-higher doses may affect heart rhythm in rare cases.
- Escitalopram (Lexapro): Similar to citalopram, but less data available. Often used as a second choice if sertraline doesn’t work.
- Venlafaxine (Effexor): Transfer rate is 1.4-5.9%. Safe for most, but watch for fussiness or sleep issues if mom’s dose is over 150mg daily.
- Mirtazapine (Remeron): Low transfer, but can cause drowsiness in babies. Sometimes used if insomnia is a major symptom.
Now, here are the ones to avoid-or use only under strict supervision:
- Fluoxetine (Prozac): This one lingers. Its active metabolite, norfluoxetine, builds up in the baby’s blood over time. One study found infant levels reaching 30% of the mother’s concentration. Not recommended unless other options fail.
- Doxepin: Linked to serious infant side effects like apnea (stopping breathing) and cyanosis (turning blue). Avoid completely.
- Bupropion (Wellbutrin): Increases seizure risk in infants. Theoretical exposure is 6-10%, and even small amounts can be dangerous in newborns.
What Side Effects Might Your Baby Actually Have?
Most babies show no reaction at all. In fact, a 2021 survey of 347 breastfeeding moms taking antidepressants found that 86% reported no noticeable effects on their infants.But for the 14% who did notice something, the most common issues were:
- Increased fussiness or crying (6.3%)
- Sleep disturbances-either sleeping too much or too little (4.1%)
- Feeding problems, like refusing the breast or taking less milk (1.6%)
- Occasional mild diarrhea or gas (rare, but reported anecdotally)
These effects usually show up in the first two weeks after starting the medication. They’re often temporary and improve with a small dose adjustment-or sometimes just time.
One mom on a Postpartum Support International forum shared: “My daughter had explosive diarrhea after I started fluoxetine. I switched to sertraline, and within 48 hours, it stopped. No more sleepless nights for either of us.”
Another said: “I thought sertraline would make my baby sleepy, but it was the opposite. He was alert, feeding well, and we bonded better than ever.”
How to Minimize Baby’s Exposure
Even with safe medications, you can reduce your baby’s exposure even further:- Take your dose right after breastfeeding. This gives your body time to clear the drug before the next feeding. Waiting 3-4 hours helps.
- Start low, go slow. Begin with the lowest effective dose. For sertraline, that’s often 25-50mg daily. You can increase later if needed.
- Monitor your baby closely for the first 2-4 weeks. Look for excessive sleepiness, poor feeding, or unusual crying. If you see any, call your doctor-but don’t stop the med on your own.
- Use LactMed. This free, science-backed database from the National Library of Medicine is updated weekly. Search any medication and get real data on transfer rates and infant effects.
What About Newer PPD Drugs Like Zurzuvae?
In August 2023, the FDA approved zuranolone (Zurzuvae)-the first pill specifically designed for postpartum depression. It works fast: half of women in trials saw symptom relief in just 15 days.But here’s the catch: the original clinical trials required women to stop breastfeeding. So official labeling says: “There are no data on the presence of zuranolone in human milk.”
Still, LactMed estimates the relative infant dose is only 0.5-1.5%-lower than fluoxetine and even some SSRIs. Experts believe it’s likely safe, but because it’s so new, most doctors recommend pumping and dumping for one week after the last dose as a precaution.
If you’re considering zuranolone, talk to a specialist. It’s expensive ($10,000+ per course), and insurance coverage is still patchy. But for moms who haven’t responded to SSRIs, it’s a game-changer-if you can manage the breastfeeding pause.

When to Call Your Doctor
You don’t need to panic over every little change. But contact your provider if your baby shows:- Extreme sleepiness-can’t wake for feedings
- Not gaining weight or refusing to feed for more than 24 hours
- Unusual jerking movements or seizures
- Blue lips or skin (cyanosis)
- Persistent vomiting or diarrhea
These are rare, but they need immediate attention. Most side effects are mild and temporary. The goal is to find a balance: enough medication to help you function, and not so much that it affects your baby.
Screening and Support Are Key
The good news? More hospitals and pediatricians are now screening for PPD. The Edinburgh Postnatal Depression Scale (EPDS)-a simple 10-question test-is recommended at 1, 2, 4, and 6 months after birth. If your score is 13 or higher, you likely have PPD.And you’re not alone. Over 78% of women in one survey continued breastfeeding while on antidepressants-and most said it made their recovery possible. Support groups, therapy, and medication work best together. Talking to a therapist who specializes in perinatal mental health can help you feel less isolated.
Remember: needing medication doesn’t mean you’re failing. It means you’re taking control. Your mental health isn’t a luxury-it’s the foundation of your baby’s well-being.
What If Medication Doesn’t Work?
If you’ve tried one or two antidepressants and still feel stuck, don’t give up. It can take 4-6 weeks for meds to fully work. If you’re still struggling after that, your doctor may:- Switch to another SSRI
- Add therapy (CBT or interpersonal therapy are most effective for PPD)
- Consider transcranial magnetic stimulation (TMS)-a non-drug option with no milk transfer
- Refer you to a perinatal psychiatrist
There are options. You just need to keep asking until you find the right fit.


Ada Maklagina
I took sertraline while breastfeeding and my kid turned into a tiny zen master. Slept like a log, ate like a champ. No drama. Just mom getting her shit together.
Lynette Myles
Zurzuvae is a pharmaceutical trap. The FDA approved it because Big Pharma paid off the regulators. No data on breast milk? That’s not safety-that’s negligence.
Michael Dioso
You think sertraline is safe? My cousin’s baby stopped gaining weight on it. They didn’t catch it until 3 months later. Doctors don’t know shit. Just push pills.
Laura Saye
There’s a profound ontological shift when maternal pharmacological intervention becomes an act of relational care rather than mere symptom suppression. The infant isn’t merely exposed to a molecule-they’re immersed in the embodied recovery of a primary attachment figure. The RID metric is reductionist; what matters is the qualitative reclamation of presence.
luke newton
So you’d rather let your baby grow up with a depressed mom who can’t even smile at them than risk a tiny bit of drug in the milk? You’re not a mother-you’re a selfish coward. This isn’t science, it’s moral cowardice.
Stephanie Fiero
you are not alone. i was there. i cried every night. i took sertraline. my baby didn’t even notice. but i started living again. you got this. don’t listen to the haters. your kid needs YOU alive and present.
Harry Nguyen
Of course the AAP says it’s fine. They’re all bought off by Big Pharma. In my day, we just drank chamomile tea and prayed. Now moms are popping pills like candy and calling it ‘self-care.’ Pathetic.
Carole Nkosi
The real issue isn’t the drug-it’s the system that makes motherhood a clinical problem to be medicated rather than a social condition to be supported. We need paid leave, childcare, and community-not another SSRIs prescription.
Manish Shankar
I am writing this with profound respect for the scientific rigor presented herein. The relative infant dose metrics are not merely statistical constructs but ethical indicators of maternal responsibility. I commend the inclusion of LactMed as a resource of unparalleled scholarly utility. It is imperative that healthcare providers disseminate such data with precision and compassion.
Chris Brown
I find it deeply troubling that anyone would suggest that pharmaceutical intervention is preferable to holistic, spiritually grounded healing. There is a moral decay in our society when we prioritize chemical solutions over prayer, discipline, and the sacred duty of maternal endurance. This article is not guidance-it is surrender.