Why generic medicines are a prime target for counterfeits
Generic drugs make up 90% of all prescriptions in the U.S., but they account for just 22% of total drug spending. That mismatch is no accident. Manufacturers of branded drugs invest heavily in packaging security - holograms, color-shifting ink, serial numbers - because their reputation and profits depend on it. Generic manufacturers? Not so much. With thinner margins and less brand pressure, many cut corners on security features. This creates a perfect opening for counterfeiters. According to the World Health Organization, up to 10% of medicines worldwide are fake, and in some regions, that number jumps to 30%. The problem isn’t just about stolen profits - it’s about lives. Fake metformin can cause kidney failure. Counterfeit antibiotics can lead to deadly resistance. A single batch of fake insulin has killed patients in multiple countries.
What to look for: Overt security features on packaging
You don’t need a lab to spot some fakes. Start with the basics. Hold the box under a regular light and tilt it. Genuine packaging often uses Optically Variable Ink (OVI) that shifts color - like green turning to blue on Pfizer’s Viagra boxes. If the color stays flat, it’s suspect. Check for holograms. Real ones have micro-text you can’t copy with a printer. Look closely: if the image looks blurry, pixelated, or doesn’t change when you move it, it’s likely fake. Examine the font. One pharmacist in Ohio caught a counterfeit version of Nexium® because the expiration date font was slightly narrower than the real one. It took three bottles before she noticed. Also check the barcode. It should be sharp, not smudged. The numbers should align perfectly with the printed text. If the barcode is too small, too large, or doesn’t scan, walk away.
Covert features: Tools that reveal hidden signs
Most counterfeiters can copy overt features. That’s why the real defense lies in covert markers. UV light is your next tool. Buy a $15 UV flashlight (365nm wavelength). Shine it on the pill bottle or leaflet. Genuine products often use invisible inks that glow under UV - white, yellow, or green. Johnson & Johnson uses this on Tylenol. If nothing glows, or it glows in the wrong color, it’s a red flag. Some packaging has RFID tags - tiny chips embedded under the label. These can’t be seen, but if you have access to a pharmacy-grade scanner, they’ll pop up in a system. Chemical taggants like Lumilink® are even harder to fake. They’re microscopic markers added to the ink. You need a handheld reader to detect them, but they’re used by major manufacturers and are nearly impossible to replicate. These aren’t for consumers - they’re for pharmacists and inspectors. But if your pharmacy has one, ask them to use it. You have a right to know your medicine is real.

Track-and-trace systems: The digital backbone of authenticity
Since 2019, the European Union requires every prescription medicine to have a unique 2D barcode with a serial number. The U.S. followed with the DSCSA, mandating full traceability by November 2023. Each package gets a unique code, linked to its batch, manufacturer, and distribution path. When you scan it, the system checks if the code is valid and hasn’t been used before. Sounds foolproof? Not quite. A 2023 study found that 35-45% of generic medicines still lack consistent serialization. Some manufacturers use different formats. Others skip it entirely. That’s why apps like MediMark fail 40-50% of the time with generics. The system works best when everyone plays by the rules - and too many don’t. The good news? The EU’s verification system handles over 2.5 billion checks a year with 99.998% uptime. The U.S. system is catching up, but gaps remain. If your pharmacy uses a verification portal and says the code is valid, you’re likely safe. If it says “invalid” or “not found,” don’t take the pills.
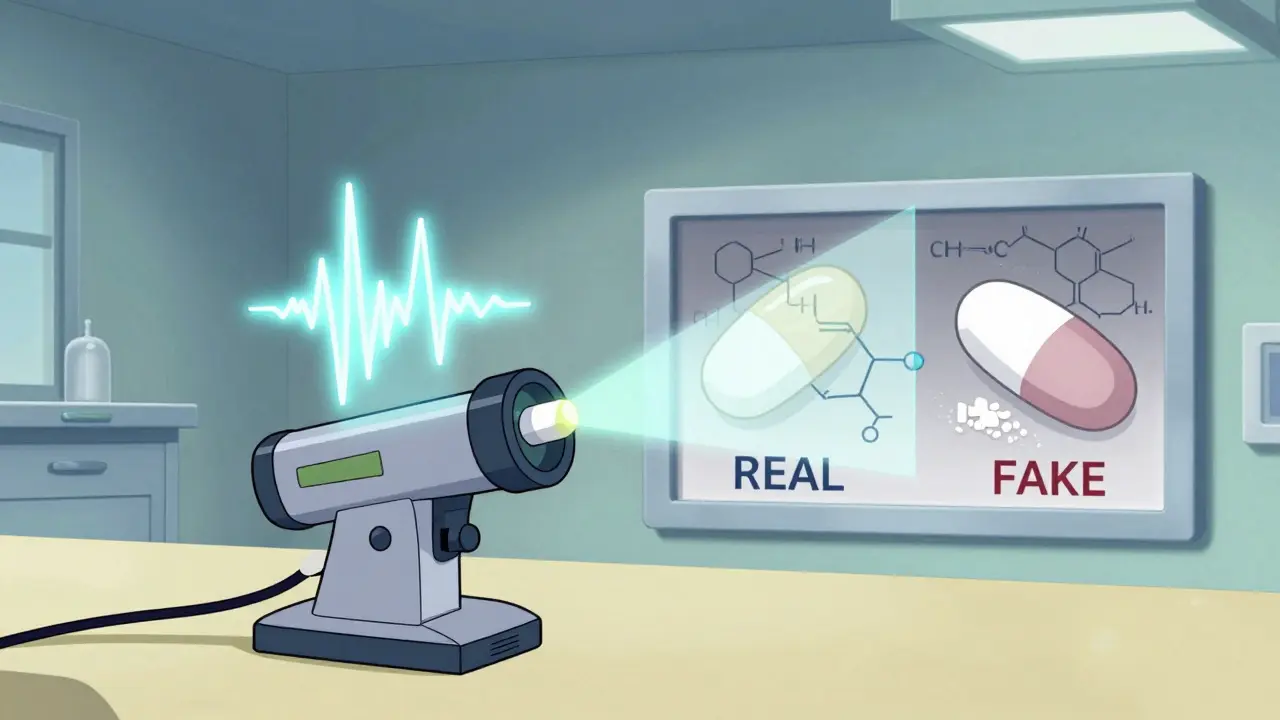
How spectroscopy detects fakes no one else can
Here’s where it gets serious. Some counterfeits look identical. Same color, same shape, same packaging. But they’re made with the wrong chemicals - maybe chalk instead of metformin, or inferior fillers. That’s where handheld spectrometers come in. Devices like the Thermo Fisher TruScan® RM or B&W Tek NanoRam® use infrared or Raman light to analyze the chemical makeup of a pill in seconds. A real metformin tablet has a unique spectral fingerprint. A fake one doesn’t match. One pharmacist in Minnesota used a NanoRam® to test a batch of generics that looked perfect. The device flagged 12 out of 50 as counterfeit. They were using sugar instead of active ingredient. The FDA’s Product Quality Research Institute says verification tools must hit 95% accuracy in real-world use. NIR spectroscopy gets 92-97% accuracy. Raman gets 88-94%. The catch? These machines cost $15,000 to $50,000. Only hospitals and large pharmacies can afford them. But if you’re on a critical drug - like blood thinners, epilepsy meds, or insulin - ask if your pharmacy has one. Many now do. And if they don’t, push for it.
Why even experts get fooled - and how to avoid it
Counterfeiters aren’t amateurs anymore. INTERPOL’s 2023 Operation Pangea report found that sophisticated fakes now replicate security features with 90-95% accuracy. That means even trained pharmacists can miss them. A 2022 survey of 1,500 U.S. community pharmacists found 68% had trouble verifying generics compared to just 22% for branded drugs. Why? Two big reasons: inconsistent labeling and lack of reference samples. If your pharmacy doesn’t have a real bottle to compare against, how can you spot the difference? The FDA’s 2023 guide says to keep authentic packaging on file. But most small pharmacies don’t. The solution? Regional verification centers. Twenty-two U.S. states now have them - places where pharmacists can send suspicious packages for analysis. Pfizer, Novartis, and other big players also offer free verification portals. You can upload photos of packaging or batch numbers. They respond within 24 hours. Use them. If you’re unsure, don’t guess. Call the manufacturer. Ask for their authentication hotline. It’s free. And it could save your life.
The future: AI, blockchain, and global standards
The fight against fake drugs is evolving. The FDA’s 2023 pilot using blockchain for generics achieved 99.2% accuracy in tracking pills across four distribution levels. By 2025, the EU will require cryptographic authentication on every generic medicine’s 2D code. Thermo Fisher’s new TruScan® Gen3 can scan a pill in 5 seconds with 98% accuracy. And AI is coming - algorithms that compare thousands of packaging patterns to spot anomalies no human can. But here’s the catch: none of this works if countries don’t cooperate. WHO reports that while 137 countries have verification rules, only 45% of Southeast Asian manufacturers follow them. That’s why counterfeiters thrive in supply chains that cross borders. Real progress means global standards - not just national ones. Until then, your best defense is layered: check the packaging, use UV light, ask about serialization, and if you’re on a life-saving drug, demand spectroscopic verification. Don’t assume it’s safe because it’s cheap. Fake medicine doesn’t care about your budget.
What you can do today
- Always inspect packaging - tilt, shine light, check fonts and barcodes.
- Use a $15 UV flashlight to look for hidden glowing marks.
- Ask your pharmacist if they use a verification system or spectrometer.
- If a barcode doesn’t scan or says “invalid,” refuse the medicine.
- Keep a photo of your real prescription bottle for comparison.
- Use manufacturer verification portals - Pfizer, Novartis, and others offer free services.
- Report suspicious drugs to your national drug regulator (like the FDA or Medsafe in New Zealand).
Counterfeit drugs are a silent threat. They don’t scream. They don’t explode. They just don’t work - or worse, they harm. But you’re not powerless. With a little knowledge and a few simple tools, you can spot the difference. And that difference? It’s everything.
How can I tell if my generic medicine is fake just by looking at the packaging?
Start by checking for color-shifting ink - tilt the box under light and see if the color changes. Look for holograms that have sharp, 3D-like details and change as you move them. Compare the font size and spacing of text - especially the expiration date - with a previous bottle. Smudged, blurry, or misaligned barcodes are red flags. If the packaging feels flimsy or the seal is loose, it’s likely counterfeit. Even small differences like a slightly different shade of blue or a misplaced logo can signal a fake.
Do UV lights really work to detect counterfeit drugs?
Yes, but only if the genuine product has UV-reactive ink. Many manufacturers, like Johnson & Johnson and Pfizer, embed invisible markings that glow under 365nm UV light. If your medicine glows in the wrong color or doesn’t glow at all, it’s likely fake. However, not all generics use this feature. Some counterfeiters now copy UV marks too, so this is just one layer. Use UV light in combination with other checks - never rely on it alone.
Can I use my phone to scan a barcode and verify my medicine?
Phone apps like MediMark or similar tools can help, but they often fail with generics. Why? Because many generic manufacturers don’t follow consistent serialization rules. The barcode might be missing, duplicated, or not registered in the system. These apps work best for branded drugs. For generics, scanning alone gives false confidence. If the app says “valid,” it’s a good sign - but if it says “invalid” or “not found,” don’t take the medicine. Always verify with your pharmacist or the manufacturer’s official portal.
Why are generic medicines more likely to be counterfeit than branded ones?
Branded drugs have strong reputations to protect. Companies like Pfizer or Merck invest heavily in security features because their brand value is tied to safety. Generic manufacturers operate on thin margins and often skip expensive security measures like holograms, special inks, or serialization. This makes them easier targets. Counterfeiters know this and focus on generics - especially high-demand drugs like metformin, atorvastatin, or losartan. The FDA found that 68% of pharmacists struggle to verify generics compared to just 22% for branded drugs.
What should I do if I suspect my medicine is fake?
Stop taking it. Do not throw it away. Contact your pharmacist or doctor immediately. Ask them to send the packaging to a regional verification center or the manufacturer’s authentication portal. In New Zealand, report it to Medsafe (the country’s medicines regulator). In the U.S., report to the FDA’s MedWatch program. Keep the packaging and receipt. Authorities need these to track the source. Never try to return it to the pharmacy without reporting - you’re helping them catch the problem before it hurts someone else.
Are handheld spectrometers worth the cost for small pharmacies?
For small pharmacies, the upfront cost ($15,000-$50,000) is high. But if you serve patients on critical medications - like blood thinners, epilepsy drugs, or insulin - the risk of a single counterfeit batch can be fatal. A 2023 Drug Topics survey found 94% satisfaction among pharmacists using devices like the NanoRam®. One device can verify hundreds of pills a day. Many pharmacies now share equipment or partner with regional labs. The cost of one patient’s harm far exceeds the price of the machine. It’s not just an investment - it’s a safety duty.

