NSAID Risk Calculator for Heart Failure
Calculate Your Risk
Estimate how NSAIDs may affect your heart failure risk based on usage duration and personal factors
Your Results
Enter your information above to see your risk assessment
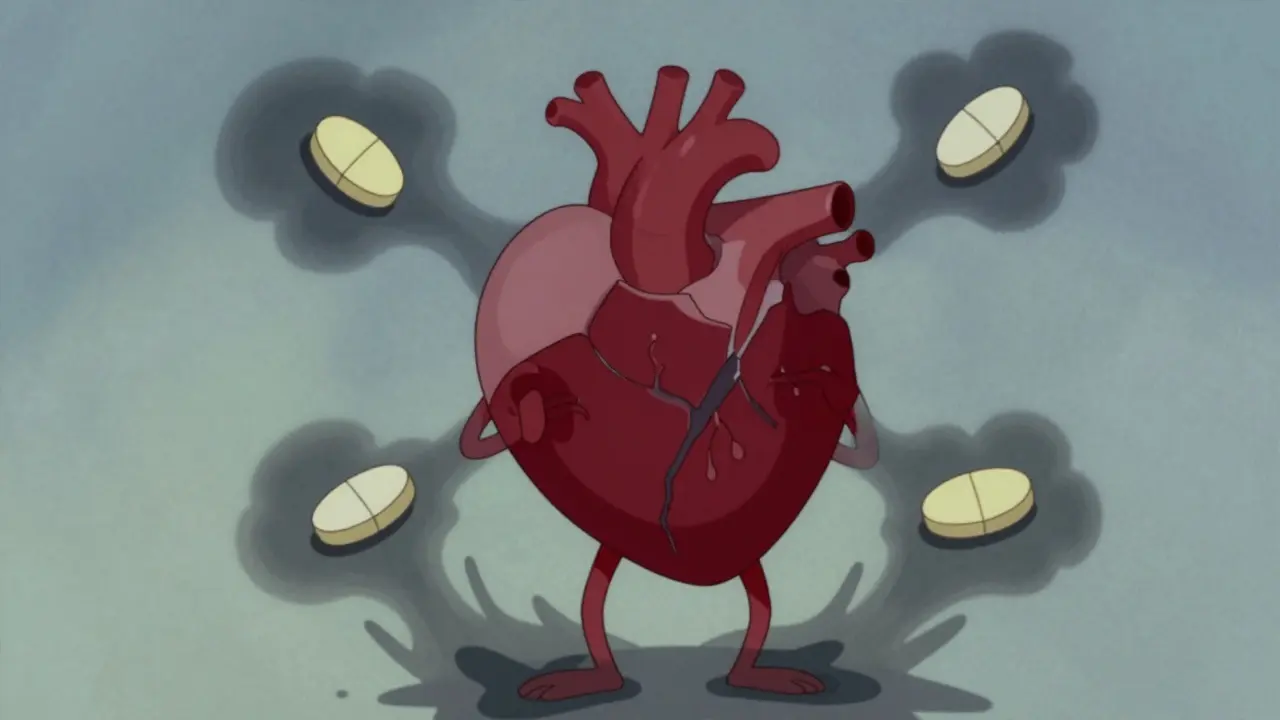
Every year, millions of people reach for over-the-counter painkillers like ibuprofen or naproxen for a headache, sore knee, or back pain. But if you have heart failure, these common drugs aren’t just harmless relief-they can push your heart into crisis. The connection isn’t theoretical. It’s proven. And it’s life-threatening.
How NSAIDs Trigger Fluid Retention
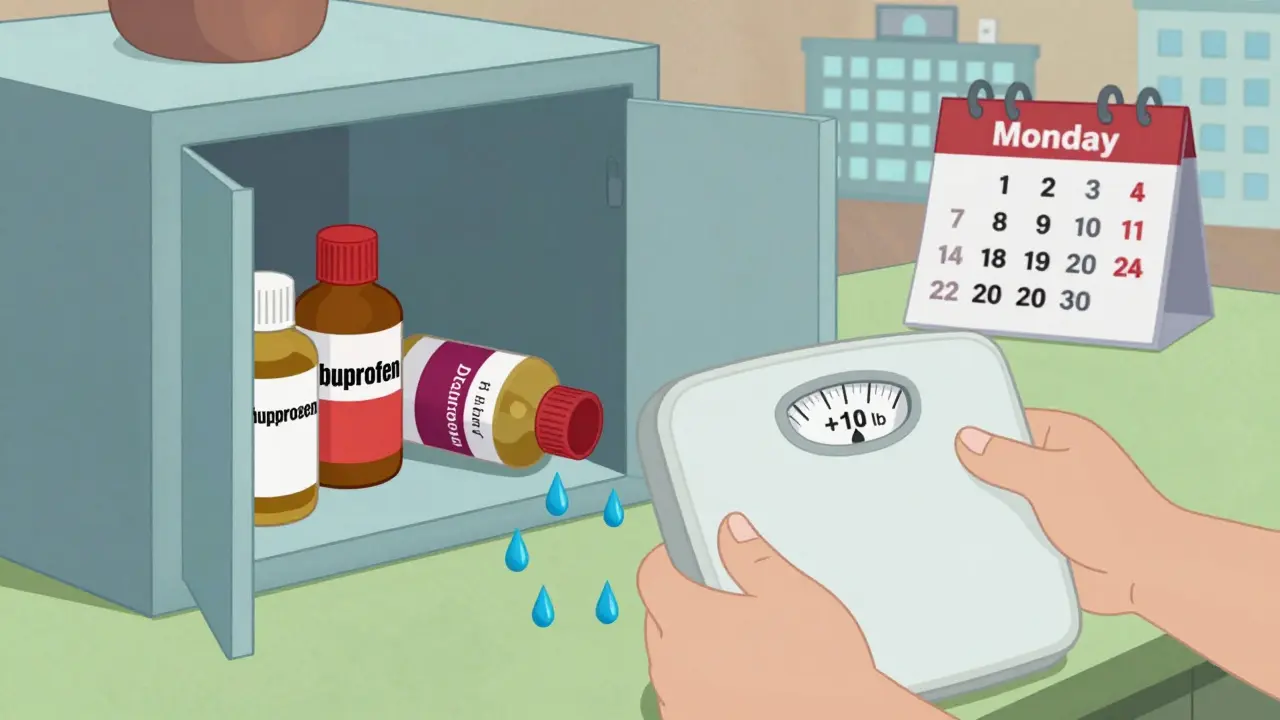
NSAIDs-non-steroidal anti-inflammatory drugs-work by blocking enzymes called COX-1 and COX-2. These enzymes help make prostaglandins, chemicals that cause pain and swelling. But prostaglandins also play a quiet, vital role in your kidneys. They help maintain blood flow and signal your body to release sodium and water. When NSAIDs shut down prostaglandin production, your kidneys start holding onto salt and fluid instead.This isn’t just minor bloating. It’s a direct hit to your heart. In heart failure, the heart is already struggling to pump blood. Extra fluid in your body means more work for a weakened organ. That extra volume raises pressure in your veins and lungs. The result? Swelling in your legs, sudden weight gain, and breathlessness even when resting. These aren’t side effects. They’re signs your heart is failing again.
Studies show this can happen fast. In one Danish study of over 100,000 people with type 2 diabetes and heart failure, even three days of NSAID use increased hospitalization risk by nearly 90%. Some patients gained over 10 pounds of fluid in just 72 hours after taking a few pills of ibuprofen. That’s not an exaggeration-it’s a documented pattern seen in clinics and emergency rooms across the world.
It’s Not Just Prescription NSAIDs
Many people think only strong, prescription NSAIDs like diclofenac are dangerous. But the real danger comes from what’s on your kitchen shelf. Ibuprofen, naproxen, and even aspirin (in high doses) are all part of this group. Celecoxib, marketed as a safer COX-2 inhibitor, carries the same risks. There’s no such thing as a heart-safe NSAID.Early hopes that COX-2 inhibitors would avoid kidney problems were wrong. Research from 2003 and confirmed by studies up to 2024 shows they reduce kidney blood flow just like older NSAIDs. The European Society of Cardiology, Medsafe in New Zealand, and the U.S. FDA all agree: no NSAID is safe for heart failure patients. The label on every bottle of ibuprofen sold in the U.S. now warns of increased heart failure risk. That warning exists because the data is undeniable.
Who’s at Highest Risk?
Not everyone with heart failure reacts the same way. The risk spikes in people over 65, those with diabetes, kidney disease, or high blood pressure. These groups already have reduced kidney function. Their bodies are less able to compensate when NSAIDs block prostaglandins. Elderly patients are especially vulnerable-many take NSAIDs regularly for arthritis, unaware of the danger.One study found that 15.7% of heart failure patients were still prescribed NSAIDs within a year of diagnosis. Among those with preserved ejection fraction (a milder form of heart failure), that number jumped to over 22%. That’s not because doctors are careless-it’s because patients often don’t tell them they’re taking OTC painkillers. A 2018 American Heart Association survey found 37% of heart failure patients used NSAIDs without telling their doctor. And 62% of those patients ended up hospitalized.
Real Stories, Real Consequences
Online forums like Reddit’s r/heartfailure are filled with posts from people who didn’t realize the risk. One man took two 400mg ibuprofen tablets for a backache. Within 72 hours, he gained 4.5 kg (10 lbs) of fluid. His legs swelled, he couldn’t lie flat, and he ended up in the ER. Another woman, told by her pharmacist that "it’s just a painkiller," took naproxen for knee pain. Two days later, she was back in the hospital with acute heart failure.These aren’t rare cases. They’re predictable outcomes of a well-documented mechanism. The body doesn’t distinguish between a pill bought at a pharmacy and one bought at a grocery store. If it’s an NSAID, it carries the same risk.
What Should You Take Instead?
The safest alternative for pain relief in heart failure is acetaminophen (paracetamol). It doesn’t affect prostaglandins in the kidneys. It won’t cause fluid retention. It won’t raise blood pressure. It doesn’t interfere with heart failure medications like diuretics or ACE inhibitors.Yes, it doesn’t reduce inflammation like NSAIDs do. But for most people with heart failure, reducing pain is the goal-not reducing inflammation. If you have arthritis or chronic joint pain, physical therapy, heat packs, or gentle movement can help more than any pill. For headaches, rest and hydration often work better than medication.
Always check with your doctor before taking anything new-even something as simple as a cold remedy. Many contain hidden NSAIDs. Some cough syrups, menstrual pain relievers, and even topical gels have ibuprofen or diclofenac in them. Your pharmacist can help you spot them.

What Doctors Should Do
Clinicians need to stop assuming patients know the risks. Only 43% of primary care doctors routinely ask heart failure patients about NSAID use during medication reviews. That’s a gap that costs lives.Guidelines from the European Society of Cardiology and the American Heart Association are clear: NSAIDs are absolutely contraindicated in all stages of heart failure. That means they shouldn’t be prescribed, recommended, or even tolerated. If a patient needs pain relief, the conversation should start with: "What are you taking for pain?" not "Have you tried anything?"
Education matters. A mobile app being developed by the American College of Cardiology, set to launch in mid-2025, will alert heart failure patients when they scan a medication barcode-warning them if it contains an NSAID. Until then, family members can help by checking labels and keeping NSAIDs out of the medicine cabinet.
The Bigger Picture
The global NSAID market is worth over $11 billion. Over 65% of sales are over-the-counter. That’s a huge industry built on convenience. But convenience shouldn’t come at the cost of heart health.Regulators have acted. Labels now warn of heart failure risk. But warnings don’t change behavior. People still buy ibuprofen because it’s cheap, fast, and familiar. They don’t realize that what feels like a quick fix could be the start of a hospital stay.
The 2024 Global Heart Failure Registry found that patients exposed to NSAIDs within 30 days of leaving the hospital had a 28% higher chance of being readmitted. That’s not just a statistic. It’s a family waiting in an ER. It’s a loved one on a ventilator. It’s a life interrupted.
There’s no gray area here. NSAIDs and heart failure don’t mix. No dose is safe. No duration is acceptable. No exception applies.
What to Do Right Now
- If you have heart failure, stop taking any NSAID unless your doctor specifically says it’s safe (and even then, it’s rare).
- Check every medicine you take-prescription, OTC, or herbal-for ibuprofen, naproxen, diclofenac, or celecoxib.
- Switch to acetaminophen for pain relief. Use it as directed, but avoid exceeding 3,000 mg per day.
- Ask your pharmacist to review all your medications for hidden NSAIDs.
- Teach your family what to look for. A spouse or child might notice a new bottle of pills before you do.
- If you’ve taken an NSAID recently and notice sudden swelling, weight gain, or trouble breathing, call your doctor immediately.
Heart failure is manageable. But it’s fragile. One pill can undo weeks of careful diet, medication, and monitoring. Don’t risk it.
Can I take aspirin if I have heart failure?
Low-dose aspirin (81 mg) used for heart attack prevention is generally considered safe in heart failure patients, because it’s used at a very low dose and for a different purpose. But higher doses of aspirin (like 325 mg) act like other NSAIDs and can cause fluid retention and worsen heart failure. Always check with your doctor before taking any aspirin, even if it’s "just for heart health."
Is naproxen safer than ibuprofen for heart failure?
Some studies suggest naproxen may have a slightly lower risk of heart attack compared to other NSAIDs, but that doesn’t mean it’s safe for heart failure. All NSAIDs-including naproxen-cause fluid retention and raise blood pressure. For heart failure patients, no NSAID is recommended. Even naproxen can trigger hospitalization. The difference in risk is small and doesn’t outweigh the danger.
How quickly can NSAIDs cause fluid retention?
Fluid retention can begin within 24 hours of taking an NSAID. Weight gain of 1-2 kg (2-4 lbs) in 2-3 days is common in susceptible patients. Some report 4-5 kg (9-11 lbs) in less than a week. Symptoms like swollen ankles, tight shoes, or shortness of breath at rest should be treated as a medical emergency.
Can I use topical NSAID creams or gels?
Topical NSAIDs like diclofenac gel or ibuprofen cream are absorbed through the skin, but they still enter your bloodstream. Studies show they can raise blood levels enough to affect kidney function and cause fluid retention, especially in older adults or those with poor kidney health. They’re not a safe alternative. Stick to acetaminophen or non-medication pain relief methods.
What should I do if I accidentally took an NSAID?
If you took one or two doses and have no symptoms, monitor yourself closely for the next 48 hours. Watch for swelling in your legs, sudden weight gain, or trouble breathing. If you notice any of these, contact your doctor immediately. If you’re on diuretics, you may need a higher dose temporarily. Never wait to see if symptoms get worse. Early action can prevent hospitalization.
Why do some doctors still prescribe NSAIDs to heart failure patients?
Some doctors may not be fully aware of the latest guidelines, or they may believe the patient’s pain is severe enough to justify the risk. Others assume the patient isn’t taking OTC NSAIDs and don’t ask. But current guidelines from the American Heart Association and European Society of Cardiology are clear: NSAIDs are contraindicated. If your doctor prescribes one, ask for evidence that it’s safe for your specific condition-and get a second opinion if needed.

Aboobakar Muhammedali
I never realized how dangerous these painkillers could be for my dad. He’s been taking ibuprofen for his arthritis for years and just last month he ended up in the hospital with fluid buildup. I wish I’d known this sooner. I’m going to throw out every bottle in the house tomorrow.
Thanks for laying it out so clearly. This isn’t just medical advice-it’s lifesaving.
Laura Hamill
THE GOVERNMENT AND PHARMA ARE LYING TO YOU!!!
Acetaminophen is just as bad but they don’t tell you because it’s cheaper and they own the patents!!
Look up Project MKUltra and the FDA’s secret meetings in 2012!!
They want you dependent on pills so you stay weak and don’t question authority!!
STOP TAKING ANYTHING!! JUST DRINK COLD WATER AND PUT ICE ON YOUR KNEES!!
❤️✊
Alana Koerts
So what? You’re telling people not to take ibuprofen but not giving them a real alternative for chronic pain. Acetaminophen doesn’t touch inflammation. People with arthritis need something that works.
Also, 90% hospitalization increase? Based on what sample size? One study? That’s not science, that’s fearmongering.
And why are you ignoring the fact that most heart failure patients are on diuretics already? Fluid retention is managed. This feels like an overreaction.
Dikshita Mehta
Thank you for this. I’m a nurse in Delhi and I see this every week-elderly patients come in with swollen legs after taking ‘just one pill’ for back pain. They don’t know the difference between ibuprofen and paracetamol.
My advice to patients: always check the active ingredient. If it says ‘ibuprofen’, ‘naproxen’, or ‘diclofenac’, put it down. Acetaminophen is your friend. So are heat packs, gentle yoga, and talking to your doctor before taking anything.
And yes, topical gels are risky too. I’ve seen cases where patients applied them daily and still ended up with fluid overload.
Education is the real medicine here.
Guillaume VanderEst
My uncle took naproxen for his knee after his heart failure diagnosis. He thought it was fine because it was ‘natural’. Two weeks later, he was on oxygen.
It’s wild how we treat pain like it’s just a minor annoyance. But for someone with a weakened heart, it’s like pouring gasoline on a fire.
I’ve started keeping a list of safe meds in my wallet now. Even my pharmacist was surprised I knew what to look for.
Thanks for the reminder. This needs to be shouted from rooftops.
Alisa Silvia Bila
Just switched to acetaminophen. No more swelling. No more panic.
Simple. Effective.
Do this.
Frank Drewery
This is the kind of post that makes me believe people still care about real health, not just quick fixes.
I’ve got a friend who’s been in and out of the hospital for heart failure. She told me last week she was ‘just taking a little ibuprofen’ for her hands. I didn’t say anything at the time. Now I’m texting her this article.
Thank you for speaking up. Someone needed to.
jessica .
THEY WANT YOU TO THINK ACETAMINOPHEN IS SAFE BUT IT’S NOT!!
It’s linked to liver damage and the FDA is hiding it!!
And why are they pushing this now? Just before the election? Coincidence? I think not.
They’re trying to control what you take so you stay dependent on the system.
Try turmeric. Or better yet-stop taking pills altogether. Your body can heal itself if you just believe.
THEY DON’T WANT YOU TO HEAL. THEY WANT YOU TO BUY.
Ryan van Leent
Why are people still taking NSAIDs? It’s not rocket science. The label says right on the bottle ‘may worsen heart failure’. If you’re dumb enough to ignore that, you deserve what happens.
And don’t even get me started on the people who say ‘but my doctor prescribed it’-your doctor is probably lazy or outdated.
Stop being a victim. Read the damn label.
Sajith Shams
Everyone’s acting like this is news. It’s been known since the 90s. I’ve been telling my cousins in Mumbai for years not to touch ibuprofen. You think your heart is fine? You’re not 25 anymore.
Acetaminophen is fine if you don’t overdose. But you’ll still die if you take 10 pills a day. This isn’t about NSAIDs-it’s about people being irresponsible.
And don’t blame the pharma companies. Blame the idiots who don’t read the fine print.
Also, topicals? Still absorb. I did the lab work. It’s not magic.
Chris Davidson
Heart failure patients should be banned from buying OTC meds. This isn’t a public health issue-it’s a personal responsibility issue. If you can’t follow basic medical advice, you shouldn’t be allowed to self-medicate.
Why are we letting people kill themselves with pills they buy at the gas station? Someone should be held accountable.
Isabel Rábago
I’m so tired of people treating heart failure like it’s something you can just ‘manage’ with a pill.
You don’t get to pick and choose which warnings to follow. If your heart is failing, you’re not ‘a little sore’-you’re fragile.
And no, your grandma’s ‘natural remedy’ of ginger tea won’t help. It’s not about what feels good. It’s about what won’t kill you.
Stop romanticizing pain. Stop glorifying ‘toughing it out’. This isn’t a movie. This is your life.
Anna Sedervay
It is, indeed, a profoundly concerning paradigmatic failure of the modern pharmaceutical-industrial complex, wherein the commodification of analgesia has superseded the primacy of patient safety. The normalization of NSAID consumption among elderly populations with comorbid cardiovascular pathology represents not merely a clinical oversight, but a systemic moral collapse.
One must question the epistemological foundations of OTC drug regulation when the very pharmacokinetic profiles of these agents are insufficiently communicated to the layperson, who, by virtue of their socioeconomic position, is often ill-equipped to interpret medical jargon.
Furthermore, the absence of mandatory visual warning systems on packaging-akin to those on tobacco products-is a glaring lacuna in public health policy.
One wonders whether the FDA’s reluctance to enforce stricter labeling stems from lobbying pressure or institutional inertia.
And yet, we persist in our complacency.
Perhaps, then, the true diagnosis is not heart failure-but societal negligence.
Matt Davies
I’ve been telling my mates for years: if your heart’s on the fritz, don’t touch the blue pills.
My mate Dave took a couple of ibuprofen for a stiff neck and ended up in ICU with his legs the size of tree trunks. He’s lucky he’s still here.
Now we all keep acetaminophen in the cupboard like it’s gold. And we check every bloody bottle-even the ones for period pain. Turns out, half of them have NSAIDs hidden in the fine print.
It’s not about being scared. It’s about being smart.
Thanks for the reminder. This needs to be on every pharmacy shelf, not just in some long blog post.
Dikshita Mehta
Just saw someone say ‘acetaminophen causes liver damage’-yes, if you take 10x the dose. But that’s true for *everything*. Salt can kill you too. The issue isn’t the drug-it’s the dosage and awareness.
For heart failure patients, acetaminophen is still the safest option. Not perfect. Not magic. But the best we’ve got.
And if you’re using NSAIDs because ‘I need the anti-inflammatory’-ask yourself: is inflammation the real problem? Or is it just pain? Most times, it’s pain. And pain can be managed without killing your heart.