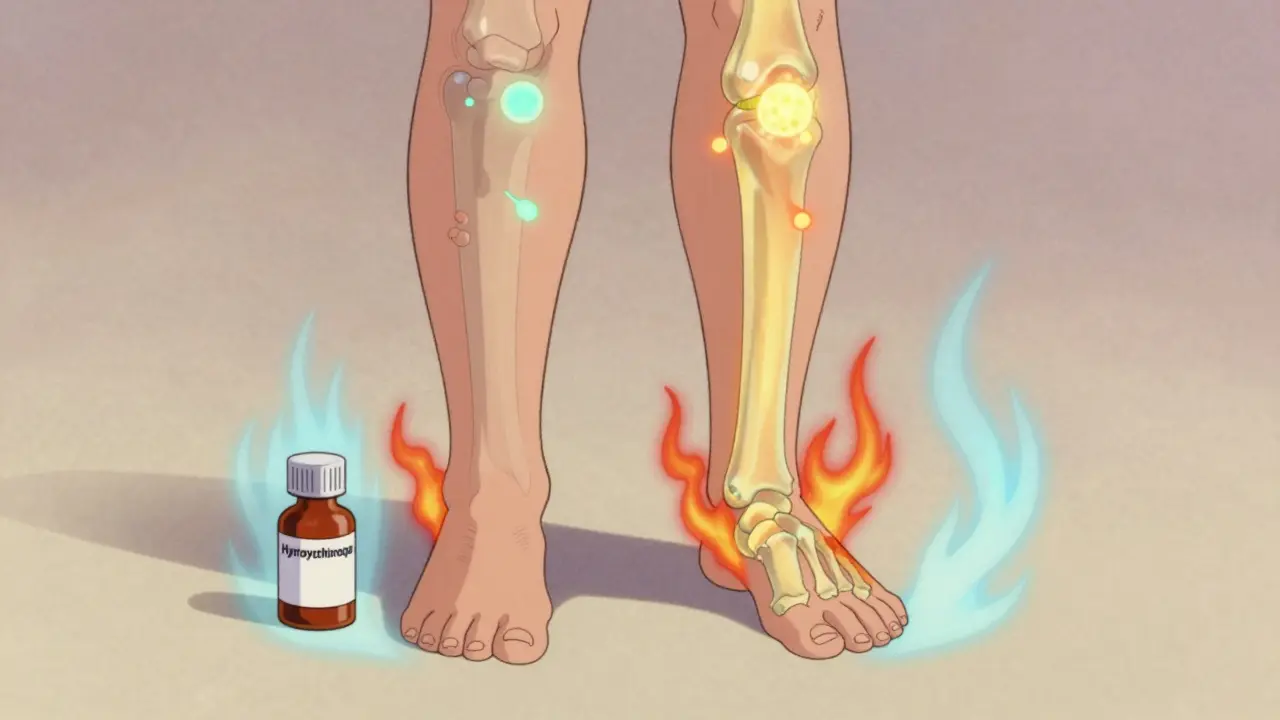
When you have lupus, your immune system doesn’t just attack foreign invaders-it turns on your own body. For about 9 out of 10 people with systemic lupus erythematosus (SLE), that means chronic joint pain, swelling, and stiffness. This isn’t just ordinary arthritis. It’s lupus arthritis, a hallmark symptom that can make even simple tasks like opening a jar or walking up stairs feel impossible. And while steroids and biologics get a lot of attention, the real backbone of treatment for most patients isn’t flashy or expensive-it’s a decades-old drug called hydroxychloroquine.
Why Hydroxychloroquine Is the First-Line Treatment for Lupus Arthritis
Hydroxychloroquine, sold under the brand name Plaquenil, isn’t a new drug. It was first made in 1946 as an antimalarial. But in the 1950s, doctors noticed something strange: patients with lupus and rheumatoid arthritis who took it for malaria seemed to feel better. That accidental discovery changed the course of autoimmune disease treatment. Today, 85-90% of SLE patients are prescribed hydroxychloroquine. Why? Because it’s one of the few drugs that doesn’t just mask symptoms-it actually slows the disease. Unlike corticosteroids, which bring quick relief but damage bones and organs over time, hydroxychloroquine works quietly in the background to calm the immune system. It doesn’t cure lupus, but it keeps flares from getting worse. The European League Against Rheumatism (EULAR) gives it the highest recommendation grade-A-for all SLE patients, no matter how mild their symptoms. That’s rare. Most drugs are only recommended for severe cases. Hydroxychloroquine is recommended for everyone because it does more than just help joints. It lowers the risk of blood clots, improves cholesterol, and cuts the chance of dying from lupus by nearly half.How Hydroxychloroquine Actually Works in the Body
It’s not magic. Hydroxychloroquine targets the immune system at the molecular level. Inside your cells, there are tiny compartments called endosomes. These are where immune cells normally detect viruses and bacteria. But in lupus, they get confused. They start reacting to your own DNA and proteins as if they’re threats. Hydroxychloroquine slips into those endosomes and blocks key sensors called TLR7 and TLR9. These sensors normally trigger inflammation when they detect trouble. In lupus, they’re stuck on high alert. By turning them down, hydroxychloroquine reduces interferon production by 35-40% and cuts TNF-alpha, a major inflammatory signal, by 25-30%. That’s why joint swelling and morning stiffness improve over time. It also messes with other pathways. It reduces the release of interleukin-1β and interleukin-6-two cytokines that fuel joint damage. It lowers reactive oxygen species (ROS) by 30-35%, which helps protect blood vessels. And it normalizes autophagy, a cleanup process in cells that goes haywire in lupus. All of this adds up to less inflammation, less pain, and fewer flares.How Long Does It Take to Work? And Why Patience Matters
One of the biggest reasons people stop taking hydroxychloroquine is because they don’t feel better fast enough. That’s understandable. If you’re in pain, you want relief now. But hydroxychloroquine doesn’t work like ibuprofen or prednisone. It takes 3 to 6 months to show real benefits. Studies show that only 62% of patients notice improvement in joint counts by 12 weeks. By 6 months, that number jumps to 85%. A patient in a 2023 case study went from needing 10 mg of prednisone daily to zero after four months on 300 mg of hydroxychloroquine. But that didn’t happen overnight. This delay frustrates people. On forums like Reddit’s r/lupus, users say things like, “It took five months. I almost quit.” But those who stick with it often say it’s the reason they’re still able to work, exercise, or play with their kids. The drug doesn’t give instant relief-but it gives lasting stability.
How It Compares to Other Lupus Arthritis Treatments
You might wonder: if hydroxychloroquine is so good, why use anything else? Methotrexate, a common arthritis drug, works better for severe joint inflammation-but it’s harder on the liver and needs monthly blood tests. Biologics like belimumab reduce disease activity more quickly, but they cost $45,000 a year. Hydroxychloroquine? $600-$1,200 a year, even with brand-name Plaquenil. Steroids give fast results-within weeks-but they cause osteoporosis, weight gain, and diabetes with long-term use. Hydroxychloroquine does the opposite: it actually increases bone density by 3-5% over two years. That’s huge for people with lupus, who are already at higher risk for bone loss. And here’s the kicker: hydroxychloroquine cuts the risk of heart attacks and strokes in lupus patients by 44%. That’s because it improves cholesterol levels-lowering bad LDL by 10-15 mg/dL and raising good HDL by 5-10 mg/dL. No other lupus drug does that.The Big Concern: Eye Safety and How to Avoid It
The scariest thing about hydroxychloroquine is the risk of retinal damage. It’s rare-but real. About 7.5% of people on the drug for more than five years develop changes in their retina that can lead to vision loss. The good news? This risk is almost entirely preventable. The American Academy of Ophthalmology says you need a baseline eye exam within the first year of starting the drug. After that, annual checkups are enough-unless you’re over 60, have kidney disease, or are on a high dose. Dosing matters. The maximum safe dose is 5 mg per kilogram of body weight per day. For a 70 kg person, that’s 350 mg. Many doctors cap it at 400 mg, but going higher doesn’t help-it just increases risk. And here’s something most patients don’t know: not all generics are the same. A 2022 study found some generic versions led to 18% lower blood levels than Plaquenil. That’s why the American College of Rheumatology now recommends sticking with the same manufacturer if possible.

sam abas
ok but like… hydroxychloroquine was literally used to treat malaria and now we’re giving it to people with autoimmune disease because some doc in 1952 noticed a guy stopped complaining about his knees? i mean sure it works but this feels like medical folklore at this point. also i’ve been on it for 8 months and my dreams still have me fighting dragons in a laundromat.
Clay .Haeber
Oh wow. So we’re now romanticizing a 78-year-old antimalarial like it’s the holy grail of medicine? Please. It’s a Band-Aid on a grenade. You’re telling me we’ve got CRISPR, mRNA tech, and AI-driven drug discovery… and the gold standard is a drug that was literally designed to kill parasites in the jungle? I’m not impressed. I’m embarrassed for modern rheumatology.
Priyanka Kumari
I’ve been on hydroxychloroquine for 3 years now and I just wanted to say - it’s not magic, but it’s the reason I can still hold my daughter’s hand without wincing. The dreams are weird, the nausea sucks, and yes, it takes forever - but I didn’t lose my job, I didn’t end up in a wheelchair, and my joints don’t feel like rusted hinges anymore. If you’re on the fence, stick with it. Your future self will thank you.
John Pope
Let’s not forget the deeper metaphysics here - hydroxychloroquine doesn’t just inhibit TLR7/9, it forces the immune system to confront its own existential crisis. You’re not treating arthritis, you’re forcing a self-destructive organism to pause, reflect, and choose compassion over chaos. The endosome is the soul’s courtroom. And HCQ? It’s the quiet judge who says, ‘Enough.’
And yes, I’ve read the papers. And no, I’m not joking. This is spiritual pharmacology.
Gregory Parschauer
Ugh. Another one of these ‘HCQ is a miracle drug’ think pieces. Let me guess - you’ve never had a retinal scan, never read the EULAR guidelines properly, and definitely don’t know that 1 in 5 patients quit because of side effects? You’re romanticizing a drug that’s literally on the FDA’s ‘caution’ list for a reason. And don’t get me started on the generic bioequivalence mess - your ‘$600 drug’ might as well be sugar pills if your pharmacy sources it from a warehouse in Bangladesh. This isn’t healthcare, it’s wishful thinking with a prescription pad.
Avneet Singh
Hydroxychloroquine’s efficacy is statistically significant but clinically marginal. The effect size on joint counts is d = 0.38 - barely above trivial. Meanwhile, the cost of monitoring (annual retinal exams, ECGs, CBCs) and the psychological burden of long-term toxicity anxiety outweigh the benefit for low-activity SLE. We’re practicing defensive medicine disguised as preventive care. The real innovation isn’t in the pill - it’s in the placebo effect of believing in it.
Nelly Oruko
It works. I’m not a doctor. But I’ve had lupus for 12 years. I’ve been on everything. This is the only thing that kept me from becoming a ghost in my own body. Don’t overthink it. Just take it. And go to your eye doctor.
Adam Vella
While the pharmacodynamic profile of hydroxychloroquine is indeed compelling, one must consider the epistemological limitations of contemporary clinical guidelines. The EULAR recommendation is predicated upon observational cohort data, not RCTs with long-term mortality endpoints. Moreover, the reduction in cardiovascular events may be confounded by confounding variables such as improved medication adherence and lower steroid burden - not the drug itself. One must therefore approach this therapeutic paradigm with epistemic humility.