Why Your Pharmacy Keeps Asking for More Paperwork
You walk into the pharmacy with a prescription for a brand-name medication. The pharmacist checks the system, pauses, and says, "We need prior authorization for this." You’re confused. You’ve been taking this drug for years. Why now? And why does it matter if there’s a cheaper generic version available? The answer lies in a system designed to save money - but often ends up costing patients and providers far more in time, stress, and delayed care.
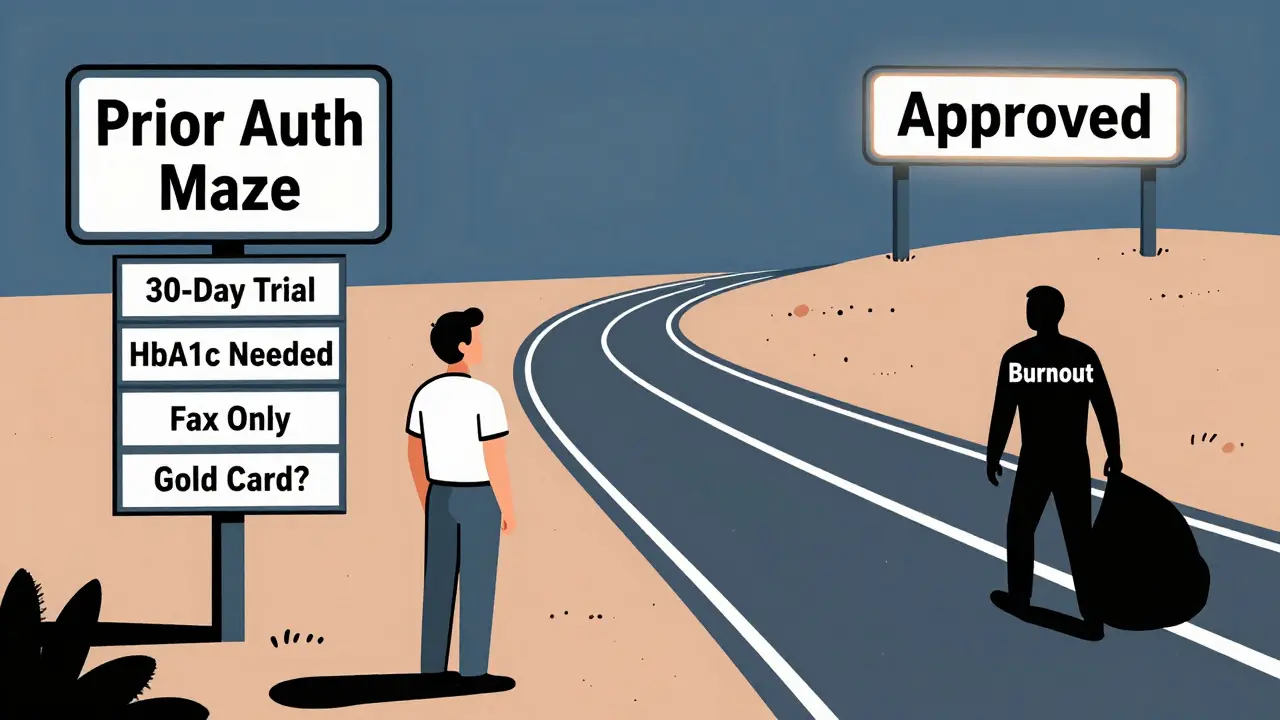
Insurance companies require prior authorization before covering brand-name drugs when an equally effective generic is available. This isn’t just bureaucracy. It’s a formalized step therapy protocol: you must try the generic first. If it doesn’t work, then - and only then - can you get the brand-name version. But getting that approval? It’s not simple. For pharmacists, it’s a daily grind of forms, phone calls, and follow-ups. For patients, it’s delays that can mean missed doses, worsening symptoms, or even giving up on treatment entirely.
How Prior Authorization Actually Works
The process starts the moment a prescriber writes a prescription for a brand-name drug. The pharmacy’s system flags it automatically if the drug is on the insurer’s list of medications requiring prior authorization. This list isn’t secret - it’s called a formulary - but it changes often, and each insurer has its own version.
Here’s the step-by-step reality:
- The pharmacy identifies the need for prior authorization based on the payer’s formulary rules.
- The prescriber must submit clinical documentation proving why the generic won’t work - not just "it didn’t work," but specifics: symptom scores, lab results, duration of trial, side effects.
- The request is submitted electronically, by fax, or over the phone - though electronic submission is now the norm for most large insurers.
- A clinical pharmacist or medical director at the insurance company reviews the request against evidence-based guidelines.
- Within 5 to 14 days (depending on the insurer), a decision is sent back: approved, denied, or needing more info.
- If denied, the provider can appeal - but that adds another 7 to 21 days.
For a simple case - say, switching from brand-name lisinopril to generic - approval can happen in hours. But for complex conditions like multiple sclerosis, rheumatoid arthritis, or mental health disorders, the paperwork can stretch to seven pages or more. And if the documentation doesn’t match the insurer’s exact wording? It gets denied. No second chances. No mercy.
Why Generics Are the First Line of Defense
Insurance companies aren’t trying to be cruel. They’re following federal guidelines and cost-saving mandates. Medicare and Medicaid require step therapy to control spending. Commercial insurers follow suit because they’re under pressure from employers and regulators to keep premiums low.
Here’s the math: generics cost 80% to 85% less than brand-name drugs. In 2023, 58% of all prescriptions filled in the U.S. were generics. But insurers still require prior authorization for 22% of brand-name prescriptions when a generic exists - meaning over 1 in 5 patients face a barrier even when a cheaper, equally effective option is available.
Step therapy rules vary wildly. UnitedHealthcare requires a 30-day trial of two different generics before approving a brand-name diabetes drug. Aetna only requires 14 days, but demands documented HbA1c readings. Cigna’s policy for hypertension allows one generic trial before approval. There’s no national standard. It’s a patchwork of rules that change with every insurer - and sometimes even within the same insurer’s different plans.

The Real Cost: Time, Stress, and Abandoned Treatments
Behind every denied prior authorization is a patient who may not get their medication. A 2024 study in JAMA Internal Medicine found that prior authorization delays cause 67% of patients to abandon their treatment - especially for mental health, diabetes, and chronic pain medications. One patient on Reddit shared that after three weeks of fighting for approval for Wegovy, she stopped trying. "I couldn’t afford to wait. My weight was getting worse, and my anxiety was worse than the cost."
For pharmacists, it’s exhausting. A 2024 survey of providers found that 68% of prior authorization requests are for generic alternatives - and they take up nearly 15 hours a week for busy clinics. That’s time that could be spent counseling patients, checking for drug interactions, or managing refills. One pharmacist in Ohio told a colleague, "I’ve spent more time on paperwork than I have with my own kids this month."
And it’s not just delays. A 2023 CMS Office of Inspector General report found that 17.3% of prior authorization denials for brand-name drugs were medically inappropriate - meaning patients were wrongly denied care because the system didn’t recognize their unique needs. That’s over 1.2 million Medicare beneficiaries annually who were stuck waiting or switched to ineffective drugs.
What Works: Real Strategies for Pharmacists
There are ways to cut through the red tape. The best pharmacists don’t just submit requests - they optimize them.
- Use payer-specific templates. Every insurer has its own form. Using their exact language and required fields cuts denial rates by 37%.
- Document failure with numbers. Saying "the generic didn’t work" gets denied. Saying "HbA1c remained above 8.5% after 6 weeks of metformin 1000 mg daily" gets approved. Specifics matter.
- Submit early. Don’t wait until the patient’s prescription runs out. Submit 14 days before the next refill is due. That’s the sweet spot.
- Go electronic. Electronic prior authorization (ePA) systems like CoverMyMeds get 78% of requests approved within the same week. Fax submissions? Only 34%.
- Know your gold card status. If your practice has a 95%+ approval rate for certain drugs, you may be "gold carded" - meaning your requests are auto-approved. But only 29% of eligible providers even know they have this status.
Some clinics now hire dedicated prior authorization coordinators. Others use automated tracking tools that alert staff when a request is stuck. One hospital system in Pittsburgh reduced approval times from 9.2 days to 2.1 days by automating documentation and using AI to pre-fill forms. First-pass approval rates jumped from 58% to 89%.
The Future: Faster, Smarter, But Still Broken
Change is coming - but slowly. Starting January 1, 2026, Medicaid managed care plans must respond to prior authorization requests in 7 calendar days for standard cases and 72 hours for urgent ones. They must also explain denials in writing. That’s a big win.
Real-time benefit tools are also being rolled out. By 2026, prescribers will see prior authorization requirements pop up on their screen the moment they type in a drug name. No more surprises at the pharmacy.
AI is helping too. Some health systems are using natural language processing to auto-generate clinical justifications from patient notes. Early results show a 44% reduction in submission time.
But the biggest threat isn’t bureaucracy - it’s burnout. A 2024 Medscape survey found 43% of physicians would reduce their patient load if prior authorization demands got worse. And 68% of them named generic alternative requests as their biggest frustration.
For pharmacists, the future means more automation, more training, and more pressure to be part doctor, part lawyer, and part IT specialist. But it also means a chance to fix a broken system - one approval at a time.
What Patients Can Do
If you’re stuck in the prior authorization loop:
- Ask your prescriber to submit the request as soon as the prescription is written.
- Call the pharmacy every 3 business days to check status.
- Ask if your insurer has a patient advocate or appeals line.
- Don’t stop your medication unless told to - sometimes, you can get a short-term supply while waiting.
- Use your insurer’s online portal to track requests. Most have real-time dashboards now.
And if you’ve been denied? You have rights. You can appeal. You can ask your doctor to write a letter of medical necessity. And you can reach out to patient advocacy groups like Patients Rising - they’ve helped thousands get approvals that insurers initially denied.
Why do insurance companies require prior authorization for generic alternatives?
Insurance companies require prior authorization for generic alternatives to enforce step therapy - a cost-control strategy that requires patients to try cheaper, equally effective generic drugs before covering more expensive brand-name versions. This is mandated by federal guidelines for Medicare and Medicaid and adopted by most commercial insurers to reduce overall drug spending. The goal is to lower costs without compromising care, but in practice, it often delays treatment and increases administrative burden.
How long does prior authorization for generics usually take?
Processing times vary by insurer. Cigna typically takes 5-10 business days, while UnitedHealthcare allows 7-14 calendar days. Starting January 1, 2026, Medicaid plans must respond within 7 calendar days for standard requests and 72 hours for urgent cases. Electronic submissions (ePA) often get approved in 24-48 hours, while fax requests can take over a week.
What happens if my prior authorization for a generic alternative is denied?
If denied, you can appeal. Your prescriber must submit additional documentation explaining why the generic failed - such as lab results, symptom logs, or documented side effects. Many denials are overturned on appeal, especially when specific clinical data is provided. You can also contact your insurer’s patient advocate or a nonprofit like Patients Rising for help navigating the process.
Can I get my brand-name drug without prior authorization?
Only if your insurer doesn’t require prior authorization for that specific drug, or if you qualify for an exception - such as a medical necessity exemption, financial hardship, or if the generic caused a severe reaction. Some insurers offer "gold carding" for providers with high approval rates, which bypasses the need for prior authorization entirely. Otherwise, you’ll need to go through the process.
Are there tools that help pharmacists manage prior authorization?
Yes. Electronic prior authorization (ePA) platforms like CoverMyMeds, Surescripts, and PDX streamline submissions and reduce denials. Many pharmacies now use automated tracking systems that alert staff when a request is pending or denied. Some clinics hire dedicated prior authorization coordinators or use AI tools that auto-fill clinical documentation from patient records - cutting submission time by nearly half.
How can I avoid prior authorization delays in the future?
Ask your prescriber to check your insurer’s formulary before writing the prescription. Submit requests at least 14 days before your current medication runs out. Use electronic submission whenever possible. Keep records of all treatment attempts with generics - including dates, doses, and outcomes. And if you’re on a chronic medication, ask if your provider is "gold carded" - that means approvals are automatic.
Final Thought: It’s Not About the Drug - It’s About the System
Generic drugs aren’t inferior. They’re the same active ingredients, tested and approved by the FDA. The problem isn’t the medication. It’s the system that treats them like a hurdle instead of a solution. Pharmacists are on the front lines of this broken process. They’re the ones holding the prescription, explaining delays, and trying to keep patients from falling through the cracks.
The system needs reform - faster decisions, clearer rules, less paperwork. But until then, the best defense is knowledge: knowing the rules, documenting everything, and never giving up on the patient’s right to timely care.


Dikshita Mehta
As a pharmacist in Delhi, I see this daily. The generics are identical, but insurers still demand 7-page forms for lisinopril. We use payer templates now-cut our denial rate by half. It’s not about the drug, it’s about the system being stuck in 2005.
pascal pantel
Let’s be real-this is just cost-shifting disguised as clinical governance. The ‘step therapy’ mandate is a corporate loophole to avoid paying for anything that isn’t dirt cheap. And don’t get me started on how ‘equally effective’ is defined by a spreadsheet, not a human. 67% abandonment rate? That’s not a statistic-it’s a crime.
Guillaume VanderEst
I had to fight for 3 weeks to get my antidepressant approved after my insurance switched me to generic. I cried in the pharmacy parking lot. My therapist said I was ‘non-compliant’ because I missed two doses. Meanwhile, the pharmacist spent 4 hours on the phone with Cigna. Who’s the real patient here?
Kevin Motta Top
Generics work. I’ve been on them for 12 years. But the paperwork? It’s designed to break you. Not the drug. Not the disease. The system. And that’s the real poison.
Carolyn Benson
Is it possible that this whole prior authorization circus is just capitalism’s way of making human suffering a line item? We treat medication like a luxury good. We punish people for needing help. And then we call it ‘fiscal responsibility.’ I’m not sure if I’m angry or just numb anymore.
Chris porto
It’s funny how we talk about generics like they’re some kind of compromise. They’re not. They’re the same molecule, same FDA approval, same science. The only difference is the price tag-and the people who get left behind because of it. We’re not saving money. We’re just moving the cost from insurers to patients’ health.
Aadil Munshi
lol so the system is broken? Newsflash. Every time I try to get my RA meds approved, I feel like I’m negotiating with a vending machine that only takes quarters from 1987. And they still won’t give me the damn thing. At least my cat doesn’t need a 14-page form to eat tuna.
Danielle Stewart
For anyone stuck in this loop: call your insurer’s patient advocate. Seriously. They’re not there to sell you insurance-they’re there to help you get your meds. I’ve helped 12 people this month get approvals after denials. You’re not alone. And you have rights.
Ryan van Leent
Why do we even have generics if we’re gonna make people jump through hoops for them? Just charge the brand price and be done with it. At least then the system wouldn’t be a joke. Also, pharmacists should just refuse to do this paperwork. Let the insurance company call the doctor themselves. It’s not their job to be clerks
Andrew Kelly
Who really benefits from this? Big Pharma? No. The insurance companies? Maybe. But the real winners? The guys writing the formulary rules. They’re paid six figures to make sure you can’t get your meds without a PhD in bureaucracy. This isn’t healthcare-it’s a surveillance state for pills.
Anna Sedervay
Let’s be honest: this entire system is a product of neoliberal austerity. The FDA doesn’t care if your HbA1c is 8.5%-they just need the paperwork to be formatted in Arial 12. And the fact that we’ve normalized this as ‘efficiency’ is the most terrifying thing about modern medicine.
Tim Goodfellow
My mate in Manchester says his NHS doc just writes the script and the pharmacy orders it-no forms, no calls, no drama. We’re in 2025 and we’re still faxing documents like it’s 1999. We’re not saving money-we’re wasting human potential. Fix the system, not the patient.
Elaine Douglass
I just want to say thank you to the pharmacists who do this every day. You’re the ones holding it all together. I know you’re tired. I see you. And I’m so grateful you never give up on us.