When your hip starts hurting, it’s easy to blame a bad workout or sitting too long. But if the pain lingers, especially when you stand up, walk, or twist, it might be something deeper-like a labral tear or early hip arthritis. These aren’t just random injuries. They’re linked, often feeding off each other, and they respond best not to rest alone, but to smart, targeted changes in how you move every day.
What’s Really Happening in Your Hip?
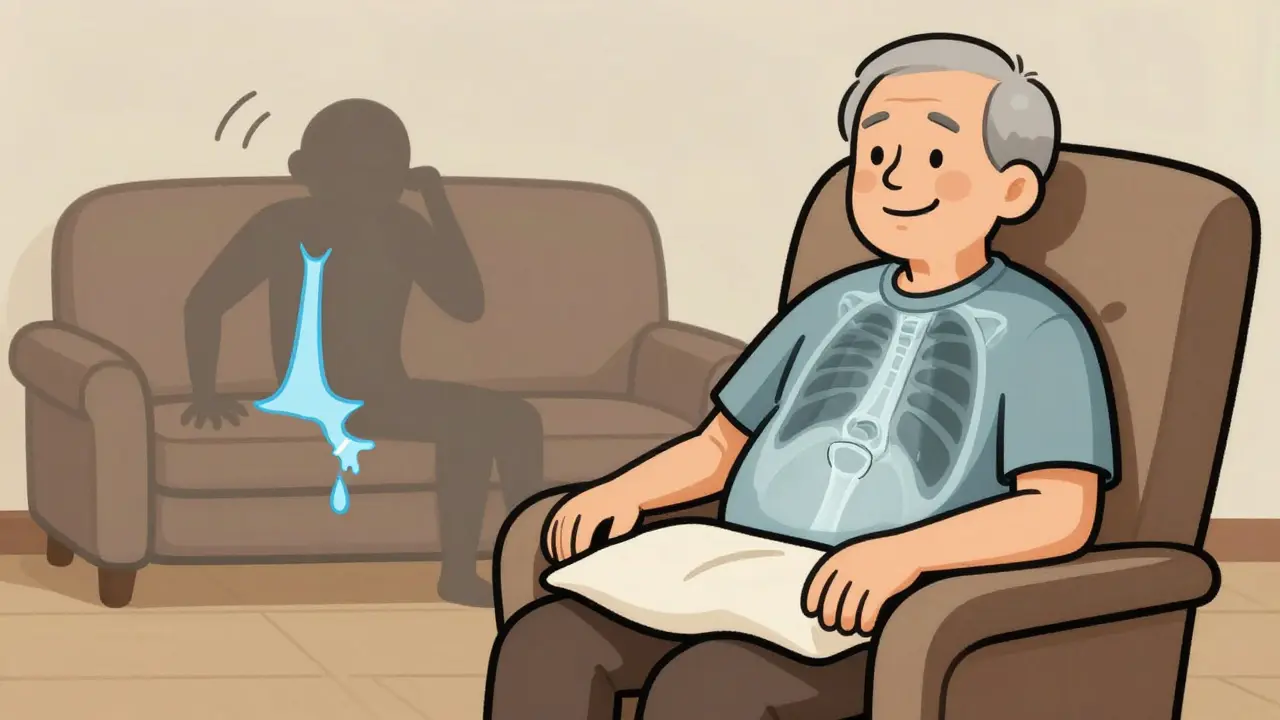
The hip joint is a ball-and-socket joint, and wrapped around the socket is a rubbery ring called the labrum. It’s about the thickness of a credit card, but it does heavy lifting: it seals the joint, holds in fluid, and keeps the ball centered. When this labrum tears-usually from repetitive twisting, deep squats, or structural imbalances like femoroacetabular impingement (FAI)-it doesn’t just hurt. It lets fluid leak out, increasing friction on the joint’s cartilage. That’s where arthritis creeps in. Hip osteoarthritis isn’t just “wear and tear.” It’s the slow breakdown of smooth cartilage that cushions the bones. When the labrum fails, contact pressure in the joint spikes by up to 92%, according to cadaver studies. That’s like driving a car with a flat tire-eventually, the rim grinds down. And once cartilage starts to thin, the body tries to repair it by growing bone spurs, which only make things worse. Here’s the catch: not everyone with a torn labrum has pain. One study found 38% of people over 50 with no symptoms had labral tears on MRI. That means the tear alone doesn’t cause pain-it’s what you do with that joint afterward. The same goes for arthritis. X-rays might show bone changes, but your pain level depends more on movement patterns than what the scan shows.Labral Tears and Arthritis: A Two-Way Street
For years, doctors thought labral tears came first, then arthritis followed. Now we know it’s messier. Arthritis can weaken the joint’s structure, making the labrum more likely to tear from normal movements. And a torn labrum can speed up cartilage loss, even in people who aren’t overweight or overly active. This is why treatment can’t be one-size-fits-all. A 35-year-old runner with a cam-type FAI (a bony bump on the femur) and a labral tear will need a different plan than a 65-year-old with advanced arthritis and a small tear. Surgery might help the first person avoid long-term damage. But for the second, surgery often doesn’t fix the root problem-widespread cartilage loss-and can lead to unnecessary recovery time. The key is identifying what’s driving the pain. If you have a sharp pain when you bend your hip past 90 degrees or rotate your knee inward, that’s likely labral irritation. If your pain is dull, deep, and worse in the morning or after sitting, it’s probably arthritis. Many people have both, and that’s where activity modification becomes your most powerful tool.Activity Modification: Not Just Resting, But Rewiring Movement
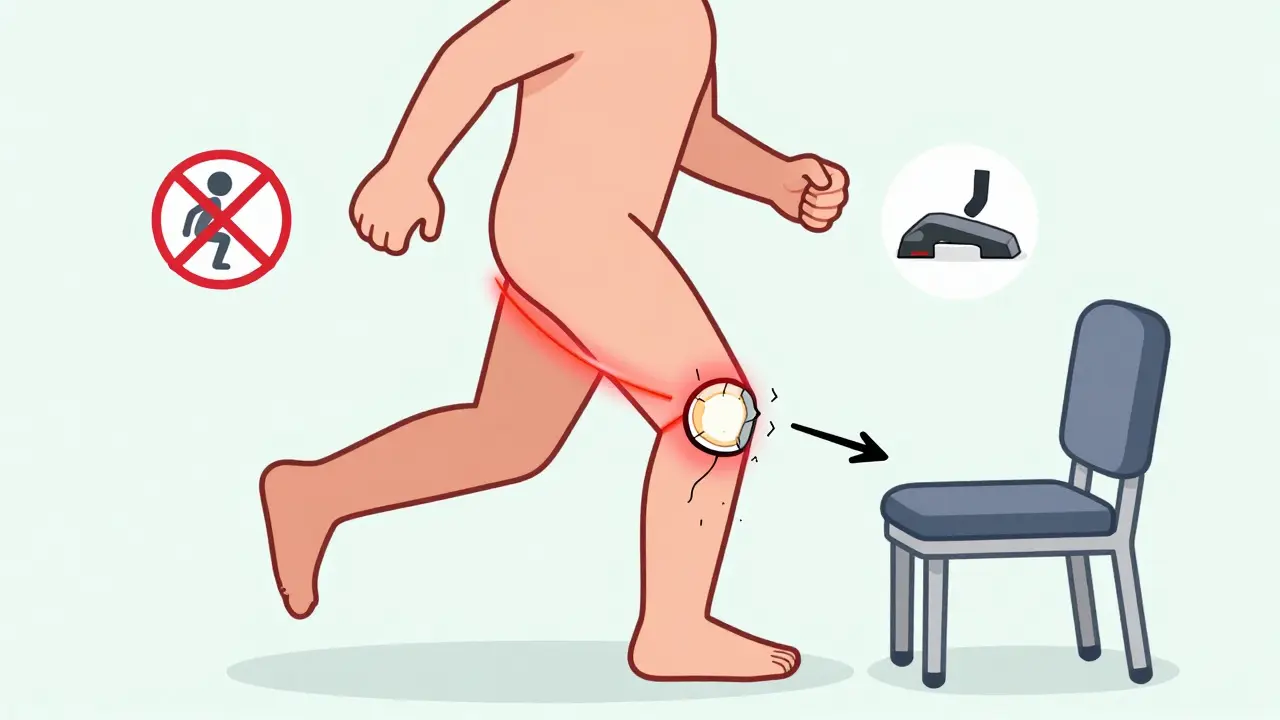
Activity modification isn’t about stopping everything. It’s about changing how you do things so you stop triggering pain. Think of it like tuning a guitar-you’re not throwing it away, you’re adjusting the strings. The Cleveland Clinic’s 2023 guidelines recommend three core rules:- Keep hip flexion under 90 degrees-no deep squats, low chairs, or sitting cross-legged.
- Avoid combining hip flexion with internal rotation-this is the “pain provocation position.” Think of twisting your knee inward while bending forward, like in pigeon pose or tying your shoes.
- Limit continuous weight-bearing to under 30 minutes at a time.
What to Avoid-and What to Do Instead
Here’s what most people with hip pain keep doing wrong:- Deep squats and lunges-These force the femur into the acetabulum at high angles, pinching the labrum. Swap them for glute bridges or step-ups with a low platform.
- Sitting in low chairs or sofas-Your hips are bent beyond 90 degrees, and your spine rounds, putting pressure on the joint. Use a cushion to raise your seat height by 2-3 inches.
- Running on hard surfaces-Impact increases joint load. Try swimming, cycling, or the elliptical instead. In one survey, 71% of people with hip pain found these alternatives sustainable.
- Standing for long periods-Shift your weight frequently. Use a footrest to alternate which leg bears the load.
When Medications and Injections Help (and When They Don’t)
NSAIDs like ibuprofen (400-800mg three times daily) can reduce inflammation and pain short-term. But they don’t fix the mechanical issue. If you’re relying on them daily, you’re masking the problem, not solving it. Corticosteroid injections give relief for about 3.2 months on average, but repeated use (more than three a year) can damage cartilage. That’s a risky trade-off if you’re trying to preserve your joint. Viscosupplementation (lubricant injections) helps about 55% of people with arthritis, but the benefit fades after six months. The new FDA-approved Durolane lasts longer-up to six months-but it’s expensive and not covered by all insurers. For most people with early-stage issues, these are stopgaps. The real solution is changing how you move. One 2023 study showed patients who focused on movement quality-learning proper alignment during daily tasks-had 40% better outcomes than those who just cut back on activity.Surgery: A Last Resort, Not a First Option
Hip arthroscopy to repair a labral tear has a 85-92% satisfaction rate at five years-for the right patient. That’s usually someone under 50 with a clear FAI deformity (alpha angle >55° on MRI), minimal cartilage loss, and good muscle strength. But if you’re over 60 with Kellgren-Lawrence Grade 3 or 4 arthritis, surgery rarely helps. In fact, 45% of those patients end up needing a total hip replacement within five years anyway. Why? Because the cartilage is already gone. Repairing the labrum won’t bring it back. The trend is shifting. The average age for hip preservation surgery dropped from 45 in 2015 to 38.7 in 2023. That’s because people are getting diagnosed earlier-thanks to better MRI tech and more awareness. But that doesn’t mean everyone with a tear needs surgery. Many can manage well with activity modification and physical therapy.Real People, Real Results
On online forums, people with hip pain share the same stories:- “I stopped running and switched to swimming. My pain vanished in six weeks.”
- “I started using a raised toilet seat. I didn’t realize how much it was hurting me just to stand up.”
- “I used to think I had to push through pain. Now I know: if it hurts, I change how I do it.”
How to Start Today
You don’t need a fancy program. Start with these three steps:- Track your pain triggers. Write down what movements make it worse-sitting, bending, twisting.
- Modify one thing this week. Swap your low chair for a higher one. Avoid deep squats. Sleep with a pillow between your knees.
- See a physical therapist who specializes in hips. They’ll teach you how to move without pain-not just strengthen muscles, but retrain your body’s habits.

Kathy McDaniel
i just started using a wedge cushion at my desk and holy crap it's been a game changer. no more morning hip stiffness. also stopped doing pigeon pose in yoga and my pain dropped like a rock. thanks for this post!
Kirstin Santiago
this is such a clear breakdown. i used to think hip pain meant i was getting old, but it's really just my movement habits. switched to swimming and raised toilet seat. no meds. no surgery. just smarter moves. life's better now.
Harry Henderson
if you're still doing deep squats and blaming your hips for pain you're literally asking for a replacement joint. stop being lazy and fix your form. this isn't rocket science. stop the nonsense and move better.
suhail ahmed
man this hits different. i used to think my hip was broken, turns out it was just screaming for respect. swapped my low couch for a throne-like chair, started sleeping with a pillow between my knees like a baby. pain? gone. felt like i got my body back. peace.
Anjula Jyala
labral tear not causing pain 38 percent of the time? that's statistically insignificant. if your MRI shows a tear and you're symptomatic you need surgery not some yoga hack. your post is dangerously misleading. cartilage doesn't regenerate. stop pretending it does
April Williams
everyone says 'just modify your movement' but nobody talks about how the medical system is rigged. insurance won't cover PT unless you're already crippled. doctors push injections because they get paid for them. you're being manipulated. this isn't health care it's a profit scheme.
Andrew Clausen
the study cited claims 71% found alternatives sustainable but does not specify the sample size or control group. without methodological transparency this is anecdotal at best. also 'raised toilet seats are not just for the elderly' is a redundant and condescending statement.
Murphy Game
they don't want you to know this but labral tears are caused by 5G radiation and the government is hiding the real cause. the real solution is magnetic resonance alignment with your chakras and avoiding fluoride in your water. the doctors are in on it.
John O'Brien
bro this is legit. i was skeptical but i did the pillow between the knees thing and now i can actually get out of bed without groaning. also swapped my running shoes for a bike. no more pain. no more pills. just simple shit that works. thank you.
Kegan Powell
the hip is like a compass man it's meant to spin and carry you through life but we treat it like a hammer. we smash it with squats we crush it with sitting we twist it till it cries. but if you just listen to it like you would a friend who's hurting? it'll guide you back. no surgery needed just presence and patience
Candice Hartley
this helped me so much 💕 i didn't even know sitting cross-legged was hurting me. changed one thing and my pain is half what it was. thank you 🙏
astrid cook
why is everyone so quick to ignore the real issue? it's not your movement it's your mindset. you're all just afraid to admit you're weak. if you were stronger you wouldn't need all these hacks. just push through like real people used to.
Paul Taylor
i've been dealing with this for years and honestly the biggest thing that changed everything was realizing i was treating my hip like a machine instead of a living part of my body. i used to think if i just worked harder i'd fix it. turns out i needed to stop forcing it and start listening. now i do glute bridges instead of squats sleep with a pillow between my knees and stand up every 25 minutes like clockwork. it's not glamorous but it's mine. i don't need a surgeon to tell me how to live. i just need to remember i'm still here and my body's trying to tell me something. it's not broken it's just asking for a little kindness. and yeah maybe that sounds soft but it's the truth. i'm 52 and i haven't had an injection in 18 months. i'm walking without pain. not because i'm young or lucky but because i finally stopped fighting myself.