Antihistamine Safety Risk Checker
This tool calculates your risk level when taking first-generation antihistamines like Benadryl, based on factors proven in medical studies. Results are based on research showing cognitive impairment can last up to 18 hours after use.
Most people reach for Benadryl when they get a rash or can’t sleep. It’s cheap, easy to find, and works fast. But what you don’t see on the bottle is how deeply it hits your brain - and how long the fallout lasts. First-generation antihistamines like diphenhydramine, chlorpheniramine, and promethazine aren’t just allergy pills. They’re powerful drugs that cross the blood-brain barrier like it’s not even there. And that’s where the real problems start.
Why These Pills Make You Feel Like a Zombie
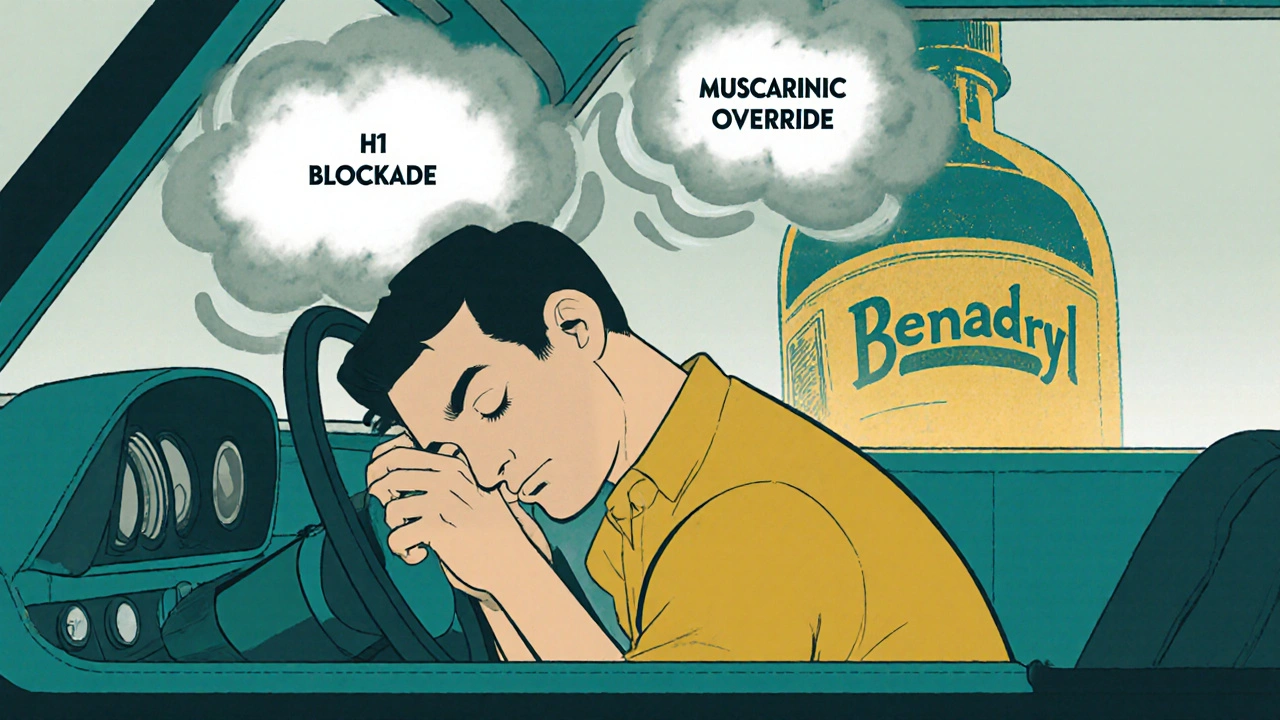
These medications don’t just block histamine. They bind tightly to your brain’s H1 receptors - but they also stick to muscarinic receptors, the same ones targeted by drugs used to treat Parkinson’s or overactive bladder. That’s why you get dry mouth, blurry vision, and trouble peeing. But the biggest issue? The drowsiness. Not the kind where you yawn and close your eyes for five minutes. This is full-on brain fog that lasts hours.
Studies show that after taking a standard 25 mg dose of diphenhydramine, brain concentrations hit 15-25 ng/mL within two hours. That’s enough to slow reaction times like alcohol. In driving simulators, users performed as badly as people with a blood alcohol level of 0.05%. And it doesn’t wear off when you think it does. Cognitive impairment can linger for up to 18 hours. That means if you take it at 8 p.m. to sleep, you might still be mentally sluggish at 2 p.m. the next day.
The Hidden Anticholinergic Toll
Anticholinergic effects aren’t just annoying - they’re dangerous, especially over time. These drugs block acetylcholine, a key neurotransmitter for memory, focus, and muscle control. In older adults, even low doses used for sleep or allergies can increase dementia risk by 54% with chronic use. That’s not a small number. It’s why the American Geriatrics Society lists first-generation antihistamines as potentially inappropriate for people over 65.
Real people report it. On forums like AgingCare.com, users say they take 12.5 mg of diphenhydramine every night to sleep. Many say it works - but 42% admit to morning confusion that lasts hours. Others describe needing artificial saliva because their mouth feels like sandpaper. Some report urinary retention so severe they needed medical help. These aren’t rare side effects. They’re predictable, documented, and avoidable.
Why Do People Still Use Them?
Because they work - fast. For motion sickness, nausea, or sudden hives, first-gen antihistamines are often more effective than newer options. Diphenhydramine cuts motion sickness symptoms by 70-80%, while second-gen drugs like cetirizine only manage 40-50%. For short-term insomnia, they reduce sleep onset by 30-40 minutes. That’s why doctors still prescribe them for these specific uses.
They’re also cheap. A bottle of 24 diphenhydramine tablets costs around $5. The same number of loratadine pills runs $15. For people without insurance or on tight budgets, the price difference is hard to ignore. And because they’re sold over the counter, many assume they’re safe. They’re not.

Who Should Avoid Them Completely?
If you’re over 65, avoid them. Period. The risk of confusion, falls, and long-term cognitive decline isn’t worth it. Even if you feel fine now, the damage builds up quietly over years.
If you drive, operate machinery, or work in a job that requires alertness - skip them during the day. The FDA has issued warnings for a reason. In 2021, 35% of emergency room visits for drowsy driving involved these medications.
If you’re on other meds, be careful. First-gen antihistamines are broken down by liver enzymes CYP2D6 and CYP3A4. If you’re taking statins, antidepressants, or even grapefruit juice, your body can’t clear them properly. Poor metabolizers - about 7% of the population - can end up with 2-3 times more drug in their system than intended. That’s a recipe for overdose.
What Are the Real Alternatives?
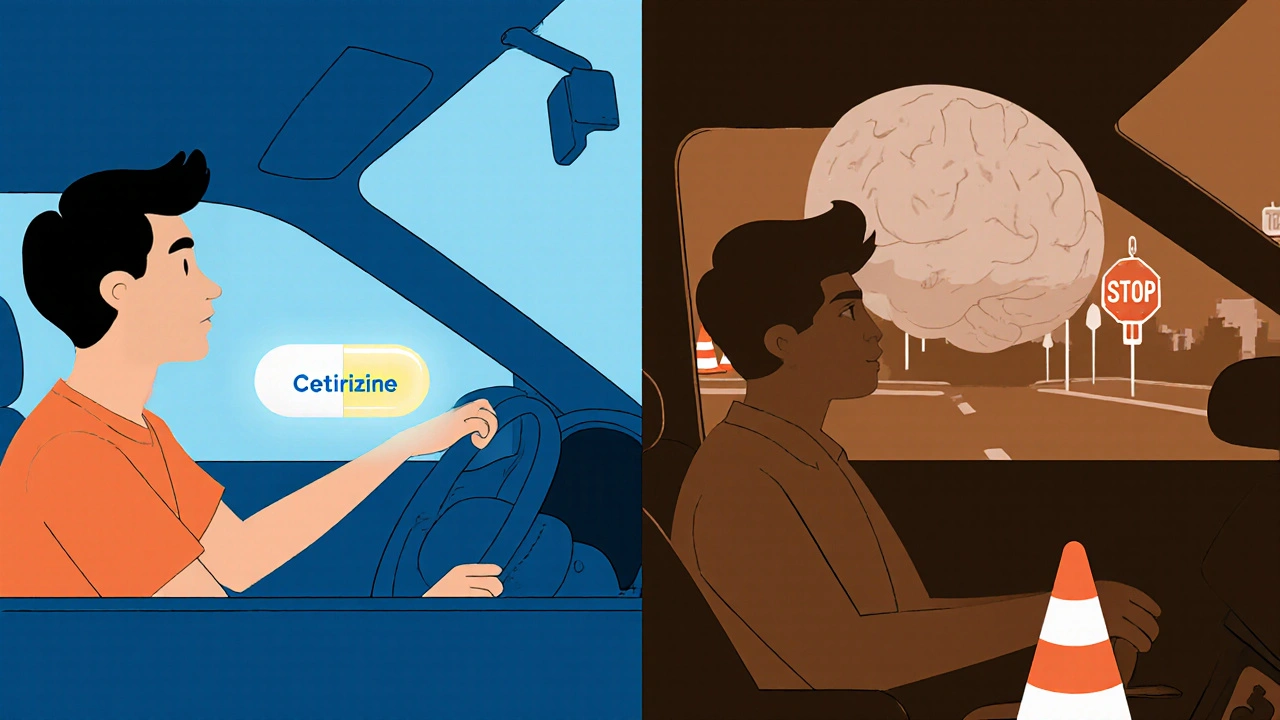
Second-generation antihistamines like cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra) don’t cross the blood-brain barrier. Their brain concentrations stay below 1 ng/mL - barely detectable. They’re just as good for allergies, last 12-24 hours, and don’t cause drowsiness in most people. Yes, they cost more. But if you’re paying for lost productivity, missed work, or worse - cognitive decline - the price isn’t just financial.
For sleep, try melatonin or behavioral fixes like reducing screen time before bed. For motion sickness, ginger capsules or scopolamine patches are safer. For nausea, ondansetron works better without the brain fog.
The Big Mistake: Thinking ‘It’s Just a Pill’
People treat these like candy. They take them before a long drive. They give them to kids for colds. They use them nightly for years. But these aren’t harmless. The FDA is already looking at restricting OTC sales of diphenhydramine after pediatric ER visits jumped 27% between 2018 and 2022. The UK banned promethazine for minors in 2022. That’s not panic - that’s science.
Even the packaging hides the truth. The small print says ‘may cause drowsiness.’ It doesn’t say ‘may leave you impaired for 18 hours.’ It doesn’t say ‘may increase your dementia risk by half.’ That’s not transparency. That’s negligence.
What to Do Instead
- Use first-gen antihistamines only for short-term, specific needs: motion sickness, acute allergic reaction, or one-time sleep aid.
- Never take them during the day unless you’re absolutely sure you can be offline for 12-18 hours.
- Never mix them with alcohol, benzodiazepines, or sleep aids. The combo can be deadly.
- For chronic allergies or insomnia, talk to your doctor about second-gen options or non-drug solutions.
- If you’re over 65, stop using them unless your doctor specifically says it’s necessary - and even then, use the lowest dose for the shortest time.
The truth is simple: these drugs are tools, not crutches. They have a place - but only in narrow, controlled situations. Outside of that, they’re outdated, risky, and unnecessary. The world has moved on. It’s time we did too.
Are first-generation antihistamines safe for long-term use?
No. Long-term use, especially in older adults, is strongly linked to cognitive decline and a 54% increased risk of dementia. These drugs have strong anticholinergic effects that accumulate over time, damaging memory and attention. They should only be used occasionally for specific, short-term needs - not as daily sleep aids or allergy treatments.
Why does Benadryl make me so sleepy?
Diphenhydramine, the active ingredient in Benadryl, easily crosses the blood-brain barrier and blocks histamine receptors in your brain that keep you alert. It also binds to muscarinic receptors, which control wakefulness and focus. This double action shuts down key parts of your central nervous system, leading to intense drowsiness that can last up to 18 hours.
Can I drive after taking a first-generation antihistamine?
No. Studies show these drugs impair driving ability as much as alcohol. Reaction times slow, attention drops, and you may not realize how impaired you are. The FDA warns against operating machinery after taking them. Even if you feel fine, your brain is still affected. Wait at least 18 hours after your last dose before driving.
Are there safer alternatives for allergies?
Yes. Second-generation antihistamines like cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra) are just as effective for allergies but don’t cross into the brain. They cause little to no drowsiness and are safe for daily use. They cost more, but they’re far safer - especially if you drive, work, or care for children.
Why are these drugs still sold over the counter?
They’re cheap, widely available, and still effective for acute conditions like motion sickness or sudden hives. Pharmaceutical companies profit from their low cost and high volume. But regulatory agencies are taking notice. The UK banned promethazine for minors in 2022, and the FDA is reviewing restrictions on diphenhydramine due to rising emergency visits, especially in children and older adults.
What should I do if I’ve been taking these for years?
Talk to your doctor. Don’t stop abruptly if you’ve been using them daily - especially for sleep. Work with your provider to switch to a safer alternative like a second-gen antihistamine or non-drug sleep strategy. If you’re over 65, this is especially urgent. Your risk of cognitive decline has already increased, and stopping now can help prevent further damage.

John Kane
Man, I never realized how much I was just living in that zombie haze after taking Benadryl for sleep. I thought I was just being lazy in the mornings, but now I get it - it’s not me, it’s the damn pill. I’ve been popping 25mg every night for years, mostly because it ‘just works.’ But reading this made me realize I’ve been sabotaging my focus at work, forgetting where I put my keys, and zoning out during conversations. I’m switching to melatonin tomorrow. No more guessing if my brain’s mine or the drug’s. Thanks for laying it out like this - I feel like I just woke up after a 10-year nap.
Callum Breden
This is the most alarmist, poorly sourced drivel I’ve read all week. You cite ‘studies’ without linking them. You mention ‘42% admit to morning confusion’ - where? On some anonymous forum? And you imply that all first-gen antihistamines are equivalent to dementia-inducing toxins. That’s not science - it’s fearmongering. Millions take these safely. My grandmother’s been on diphenhydramine for 20 years and she’s sharper than half the millennials I know. Stop weaponizing pharmacology to sell your blog.
Mansi Gupta
I appreciate the effort to raise awareness, but I think the tone might be too alarming for some readers. In India, many people rely on these medications because second-gen options are either expensive or not available in rural areas. Perhaps a more balanced approach - acknowledging the risks while offering practical, accessible alternatives - would help more people. For example, ginger for motion sickness or warm milk before bed. Not everyone can afford Zyrtec, but they can afford a cup of tea and a quiet room.
Erin Corcoran
OMG YES. I took Benadryl before a road trip last year and nearly crashed. I thought I was ‘fine’ - until my husband said I was weaving and mumbling. 😳 Now I keep a bottle of Claritin in my glovebox and a note on my phone: ‘Diphenhydramine = brain fog zone.’ Also, my mom (72) stopped hers after reading this - and she’s been sleeping better without it! 🙌 #DontBeASlaveToThePill
shivam mishra
As someone who works in pharmacy in Delhi, I see this every day. People buy diphenhydramine like candy - for colds, for sleep, for kids’ coughs. We try to warn them, but they say, ‘But it’s OTC, right?’ The real issue isn’t just the drug - it’s the lack of public health education. We need community workshops, posters in local clinics, even WhatsApp blasts in regional languages. Second-gen antihistamines are available now in most urban pharmacies at reasonable prices. It’s not about fear - it’s about awareness. And yes, if you’re over 60, please, please, please talk to your doctor before taking anything with ‘anticholinergic’ on the label. Your brain will thank you.