When you're taking a direct oral anticoagulant (DOAC) like apixaban, rivaroxaban, or dabigatran, you might think your blood thinner is simple to manage-no regular blood tests, fewer food restrictions, and less hassle than warfarin. But that doesn't mean it's safe to take with just any other pill. Even small changes in what you're on can push your DOAC levels too high or too low, leading to serious bleeding or dangerous clots. The truth is, DOAC interactions are more common than most patients and even some doctors realize.
Why DOAC Interactions Matter More Than You Think
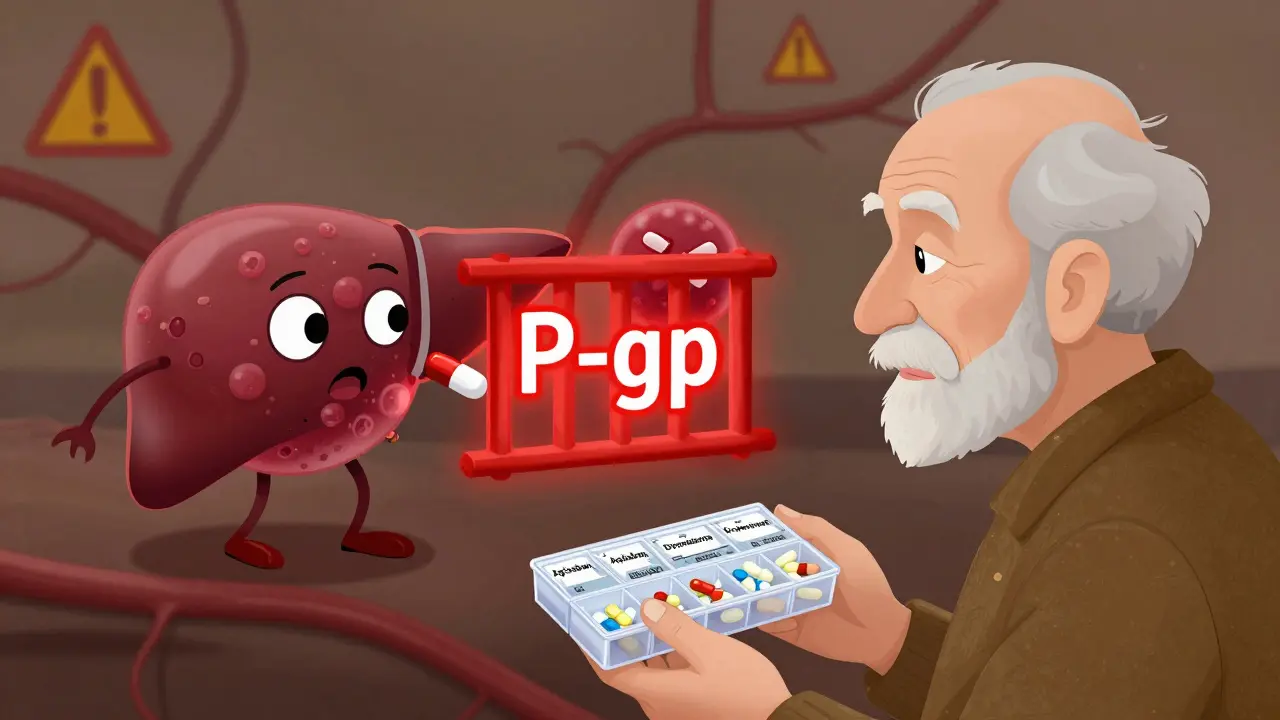
DOACs work by blocking specific proteins in your blood that help clots form. Unlike warfarin, which affects vitamin K and has hundreds of known interactions, DOACs are designed to be more predictable. But predictability doesn’t mean immunity. Their safety depends on staying within a narrow range of concentration in your bloodstream. Too little? You're at risk for stroke or pulmonary embolism. Too much? You could bleed internally without warning. Most people on DOACs are older and managing multiple conditions-high blood pressure, diabetes, heart failure, atrial fibrillation. That means they’re often taking five or more other medications. Every additional drug adds a chance for interference. A 2020 review from the American College of Cardiology found that nearly all DOAC users are on polypharmacy, making interaction risks unavoidable if not actively managed.How DOACs Are Metabolized: The CYP3A4 and P-gp Connection
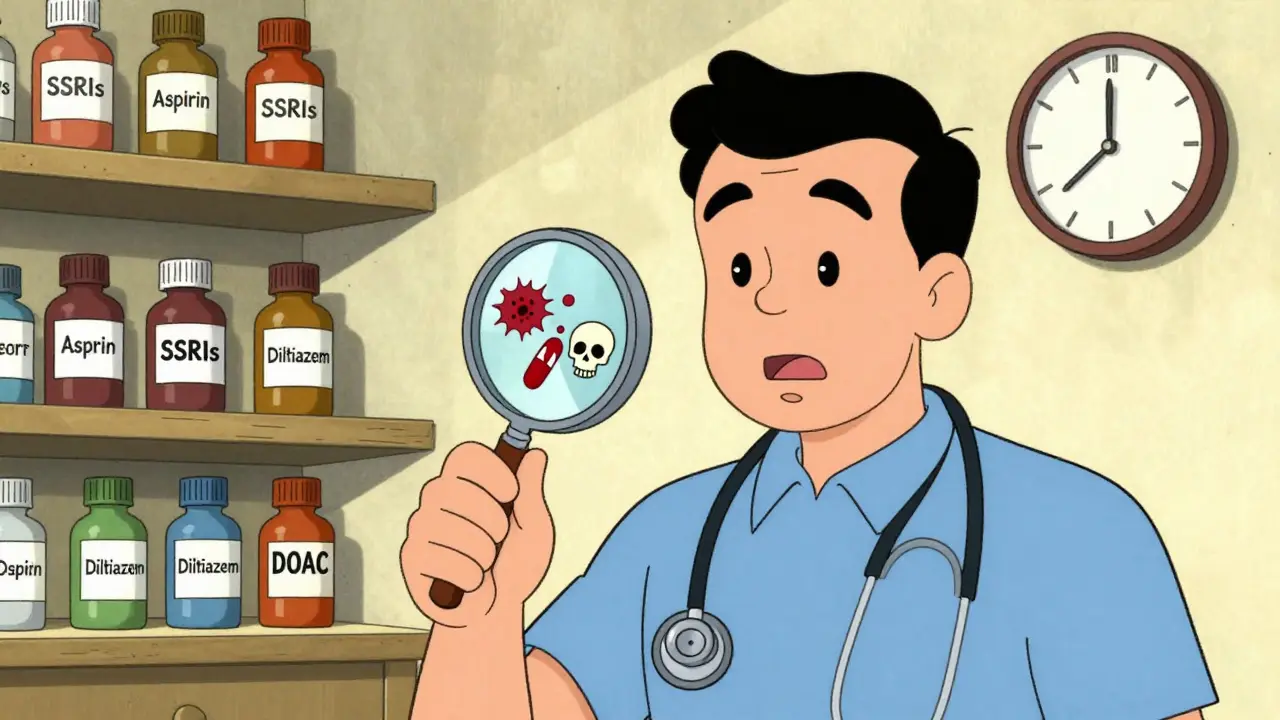
The main reason DOACs interact with other drugs comes down to two biological systems: the CYP3A4 enzyme and the P-glycoprotein (P-gp) transporter. These are like gatekeepers in your liver and intestines that control how much of a drug gets into your bloodstream. - Apixaban: About 20-25% is broken down by CYP3A4; mostly cleared by P-gp. - Rivaroxaban: Half of it goes through CYP3A4; also heavily dependent on P-gp. - Dabigatran: Almost entirely cleared by P-gp, with almost no CYP3A4 involvement. - Edoxaban: Mostly P-gp, minimal CYP3A4. - Betrixaban: Same as dabigatran and edoxaban-P-gp driven. This means drugs that block or speed up these systems can dramatically change how much DOAC stays in your body.High-Risk Medications to Watch Out For
Some medications are known troublemakers. Here’s what to avoid or adjust:- Dronedarone (for irregular heartbeat): Strongly blocks P-gp. Avoid with dabigatran and rivaroxaban. If you’re on edoxaban, your dose must drop from 60 mg to 30 mg daily.
- Amiodarone: Moderately blocks P-gp. Can raise DOAC levels. Monitor closely for bruising, blood in stool, or dizziness.
- Diltiazem: Weakens CYP3A4 and P-gp. Use with caution-especially with apixaban or rivaroxaban. Bleeding risk increases.
- Verapamil: Blocks P-gp. Dabigatran dose must be reduced to 110 mg twice daily if you’re taking it for stroke prevention. Apixaban and rivaroxaban are less affected.
- Strong CYP3A4 or P-gp inducers: Like rifampin, carbamazepine, St. John’s wort. These can slash DOAC levels by up to 50%. Never combine unless under strict supervision.
It’s Not Just Prescription Drugs
Many people forget about supplements and over-the-counter meds. These can be just as dangerous. - St. John’s wort: A common herbal remedy for depression. It’s a strong P-gp and CYP3A4 inducer. One study showed it cut rivaroxaban levels by nearly half-enough to trigger a clot.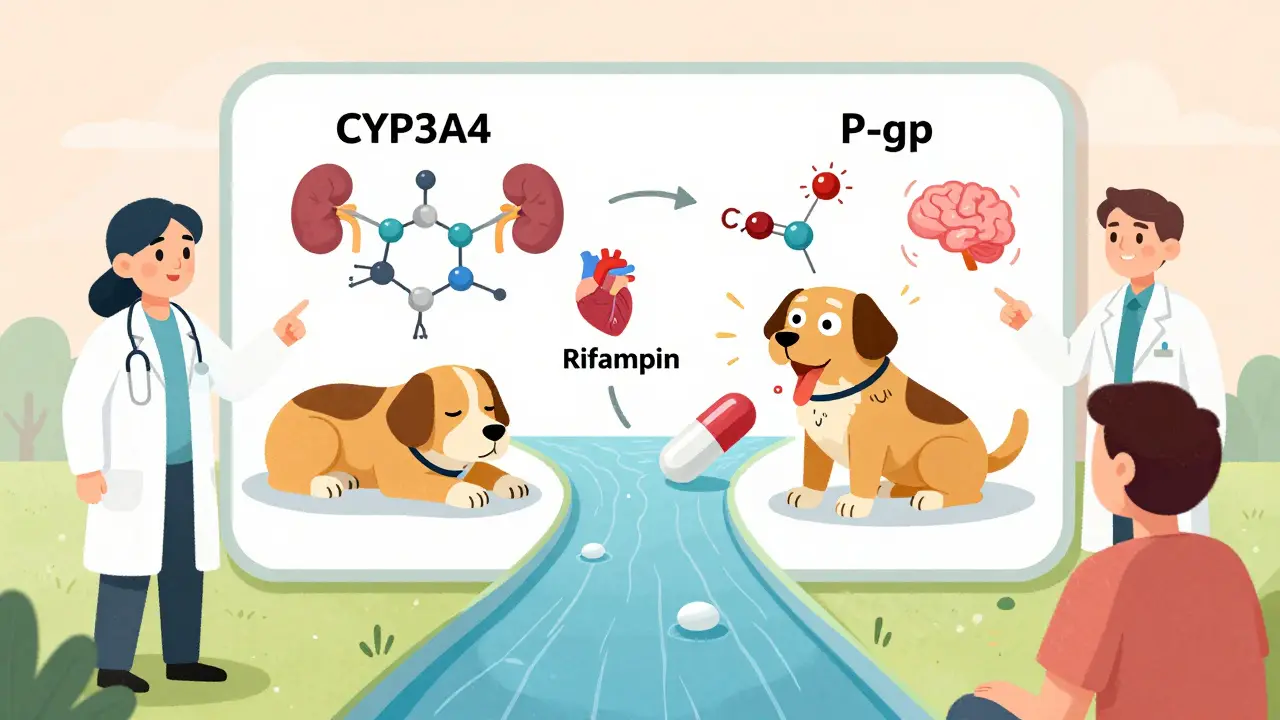
Dose Matters-Even Within the Same Drug
Rivaroxaban isn’t just rivaroxaban. The dose you’re on changes how it behaves. - If you’re taking 20 mg once daily for atrial fibrillation, it’s absorbed differently than if you’re on 2.5 mg twice daily after a heart attack. The lower dose has a higher minimum concentration (Cmin), meaning it stays in your system longer. So if you’re on the 2.5 mg regimen and start a new medication that blocks P-gp, your exposure might spike more than someone on the 20 mg dose. This isn’t just theoretical-studies show different interaction patterns based on indication.What About Kidney Function?
Your kidneys clear most DOACs. If your kidney function drops-even slightly-your body can’t remove the drug as fast. That’s why doctors lower DOAC doses in patients with moderate kidney disease. But here’s the catch: if you have reduced kidney function AND take a drug that blocks P-gp or CYP3A4, you’re hit with a double hit. Your body can’t clear the DOAC, and the other drug is forcing more of it into your blood. This combination is a recipe for major bleeding. A 2020 study in the Journal of Thrombosis and Haemostasis found that patients with both renal impairment and a P-gp inhibitor had a 3.5 times higher risk of major bleeding than those with just one risk factor.What You Should Do Right Now
You don’t need to panic. But you do need to act.- Make a full list of everything you take: prescriptions, OTCs, vitamins, herbs, even cough syrup. Bring it to every doctor visit.
- Ask your pharmacist to run a drug interaction check every time a new medication is added. Pharmacists are trained to catch these.
- Don’t start or stop anything without talking to your anticoagulation provider-even something as simple as a new pain reliever.
- Know your signs of bleeding: Unusual bruising, pink or red urine, black stools, headaches, dizziness, or unexplained swelling. Call your doctor immediately if you notice any.
DOACs vs. Warfarin: The Real Advantage
It’s true that DOACs have fewer interactions than warfarin. Warfarin is affected by vitamin K in leafy greens, alcohol, antibiotics, and dozens of other drugs. But that doesn’t mean DOACs are safe by default. It just means the interactions are less obvious. The real advantage of DOACs is consistency. No weekly INR checks. No dietary restrictions. But that same consistency means you can’t rely on lab tests to catch a problem. If a drug interaction lowers your DOAC level, you won’t know until you have a stroke. If it raises it, you won’t know until you bleed.Future of DOAC Management
Right now, we’re flying blind in many cases. We don’t have standard blood tests to measure DOAC levels in routine care. Some hospitals do specialized tests, but they’re not widely available. Experts are pushing for therapeutic drug monitoring-measuring actual DOAC concentrations in blood-to guide dosing, especially when interactions are suspected. But current evidence isn’t strong enough to make it standard practice. In the future, we may see personalized dosing based on genetics, kidney function, and interacting drugs. Until then, the best tool you have is awareness and communication.Bottom Line
DOACs are safer than warfarin-but only if you treat them with respect. They’re not "set and forget." Every new medication, supplement, or even change in your diet can change how they work. The risk of bleeding or clotting is real, and it’s often hidden until it’s too late. Stay informed. Stay proactive. And never assume your doctor knows every pill you’re taking. Be your own advocate. Keep a list. Ask questions. And never let convenience override caution.Can I take ibuprofen with a DOAC?
It’s not recommended. Ibuprofen and other NSAIDs don’t change DOAC levels, but they increase bleeding risk by irritating the stomach lining and reducing platelet function. If you need pain relief, acetaminophen (Tylenol) is safer. Use NSAIDs only if your doctor says the benefit outweighs the risk-and never for long-term use.
Is St. John’s wort safe with apixaban?
No. St. John’s wort strongly activates CYP3A4 and P-gp, which can cut apixaban levels by up to 50%. This puts you at high risk for stroke or blood clots. Stop taking it immediately if you’re on a DOAC, and tell your doctor before starting any herbal supplement.
Do I need blood tests while on a DOAC?
Routine blood tests like INR aren’t needed for DOACs, unlike warfarin. But if you have kidney problems, are taking interacting drugs, or have signs of bleeding or clotting, your doctor may order a specific anti-Xa or ecarin clotting time test to measure DOAC levels. These aren’t standard but can be lifesaving in complex cases.
What if I need surgery while on a DOAC?
Your doctor will pause your DOAC before surgery, usually 24-48 hours before, depending on the drug and your kidney function. For high-risk procedures, they may use a reversal agent like andexanet alfa (for apixaban, rivaroxaban) or idarucizumab (for dabigatran). Never stop your DOAC on your own-always follow your care team’s instructions.
Can I switch between different DOACs if one interacts with my other meds?
Sometimes, yes. For example, if you’re on rivaroxaban and need to start dronedarone, switching to apixaban may be safer because it’s less affected by P-gp inhibitors. But this isn’t automatic-it requires careful planning. Dosing differs between DOACs, and switching without adjustment can lead to under- or over-anticoagulation. Always consult your anticoagulation specialist before switching.

Katie Schoen
Honestly? I thought DOACs were the magic bullet until my grandma almost bled out because she was taking St. John’s wort for ‘anxiety’ and her pharmacist didn’t flag it. 🤦♀️ Now I carry a laminated list of meds in my wallet. Don’t be like her.
Beth Templeton
NSAIDs bad. Tylenol good. Done.
Cam Jane
I’m a nurse and I can’t tell you how many patients I’ve seen on DOACs who think ‘no blood tests’ means ‘no monitoring needed.’ Spoiler: your kidneys aren’t magic. If you’re over 65 and on three meds, you need a med review every 3 months. Not ‘when you feel weird.’ Every. Three. Months. And yes, your cousin’s ‘natural heart tonic’ from Etsy counts as a med. Bring it to the appointment.
Wesley Pereira
P-gp and CYP3A4? Yeah I know those acronyms. But here’s the real issue - docs don’t even ask about supplements. My uncle was on rivaroxaban and started turmeric capsules ‘for inflammation.’ No one checked. He ended up in the ER with a GI bleed. The doc blamed him. He didn’t even know turmeric affects P-gp. 😑
Kelly Beck
I just want to say thank you for writing this. I’m 72, on apixaban for AFib, and I take 7 meds including metformin, lisinopril, and a daily aspirin (my cardiologist says it’s okay, but I still panic). I printed this out and gave it to my pharmacist - she actually cried and said ‘this should be mandatory reading.’ I used to think DOACs were easy. Now I know they’re just quiet killers. I’ve started keeping a little notebook: meds, dates, symptoms. It’s not glamorous, but it’s keeping me alive. 🙏❤️
Isaac Jules
Wow. Another ‘DOACs are dangerous’ fearmongering post. Did you even read the FDA label? The bleeding risk is 0.5% per year. You’re more likely to die from falling in the shower. Stop scaring people into thinking their meds are landmines. Also, St. John’s wort? People have been taking it for centuries. Your ‘study’ is from 2020. So what? I’m sure your cousin’s cardiologist is also a witch.
Tiffany Adjei - Opong
Okay but let’s be real - the whole ‘DOACs are safer than warfarin’ narrative is corporate propaganda. Warfarin has been around since 1954. We know how to manage it. DOACs? We’re still guessing. No monitoring, no reversal agents available everywhere, and now we’re supposed to memorize CYP3A4 pathways? My grandma doesn’t know what ‘P-gp’ is. Neither do 90% of PCPs. This isn’t patient safety - it’s pharmaceutical convenience with a side of liability avoidance.
Dana Termini
I appreciate the detail here. I’ve been on dabigatran for 4 years. My kidney function dropped from 60 to 45 last year and my doctor didn’t adjust my dose until I brought this up. I’m glad someone’s saying it: kidney + P-gp inhibitor = double whammy. I’ve started asking every prescriber ‘does this affect P-gp?’ Now they just hand me the list. Progress?
Ryan Barr
CYP3A4? P-gp? You’re overcomplicating it. Just avoid grapefruit and don’t be a dumbass. The rest is noise.
Molly McLane
I’m a pharmacist and I want to say - if you’re on a DOAC and you’re prescribed a new medication, don’t just assume it’s fine. Bring your list. Ask: ‘Is this going to interact with my blood thinner?’ Most pharmacists will do a free interaction check right there. We’re not just pill counters. We’re your safety net. Also - if you’re on amiodarone and rivaroxaban? Please. Just please. Call your anticoag clinic. You’re one missed dose away from disaster.
Amy Le
America’s healthcare system is a joke. We give people life-saving drugs but don’t teach them how to use them. We let pharmacists do the work doctors refuse to do. We let herbal supplements fly under the radar. And then we blame patients when they bleed. This isn’t about DOACs. It’s about a system that treats people like disposable data points. 🇺🇸💀