Understanding Central Cranial Diabetes Insipidus
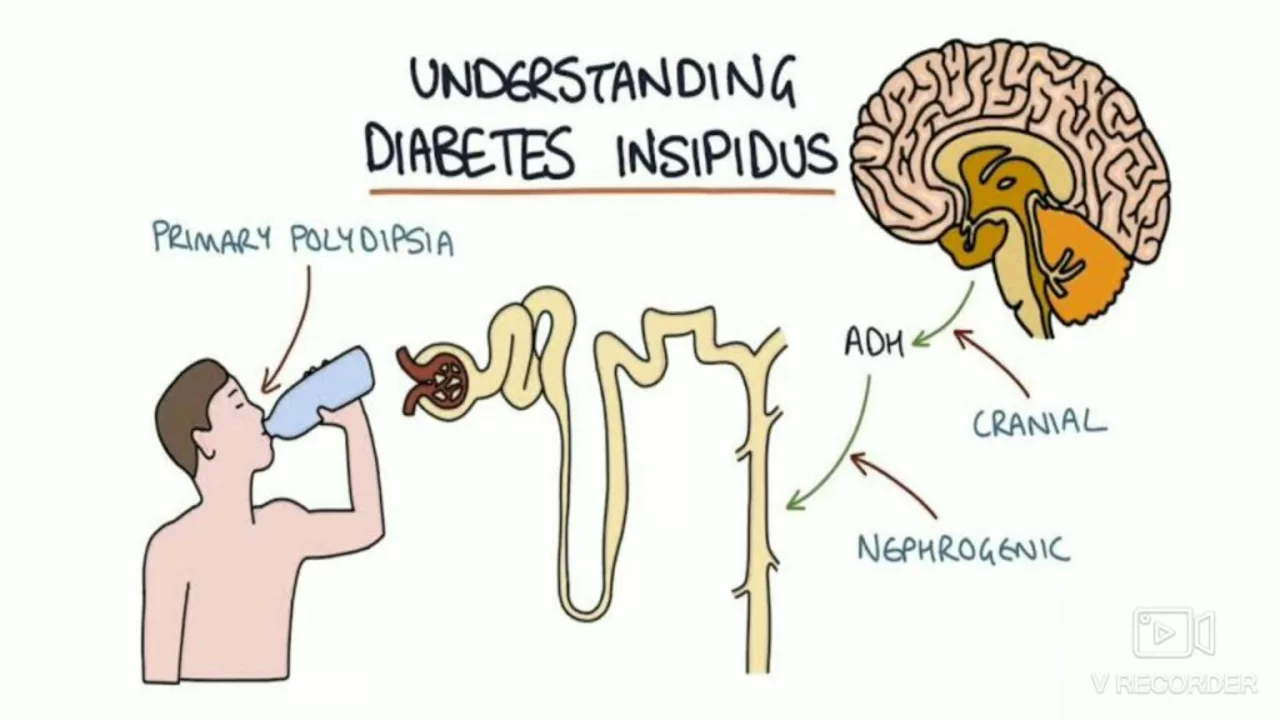
As a blogger, I've always been fascinated by the intricacies of the human body and how it operates. One of the conditions that piqued my interest recently is Central Cranial Diabetes Insipidus, a rare disorder that affects the body's ability to balance fluids. This condition results from a deficiency of the antidiuretic hormone (ADH) or vasopressin, which is produced in the hypothalamus and stored in the pituitary gland. This hormone plays a crucial role in the kidneys' regulation of water in the body. If you or a loved one has been diagnosed with this condition, this article will provide you with a comprehensive understanding of the tests and procedures involved in its diagnosis.
Initial Evaluation and Symptoms
The first step in diagnosing Central Cranial Diabetes Insipidus often involves an initial evaluation of the symptoms. Patients typically present excessive thirst and frequent urination, particularly at night. They may also experience dehydration, dry mouth, and fatigue. As I delved deeper into the condition, I discovered that these symptoms can be quite taxing on the patients and significantly affect their quality of life.
Medical History and Physical Examination
The next crucial step in diagnosing Central Cranial Diabetes Insipidus is a thorough medical history and physical examination. During this process, the healthcare provider will ask about your symptoms, any existing medical conditions, and any medications you are currently taking. They will also conduct a physical examination to check for signs of dehydration and other related complications.
Urine and Blood Tests
One of the primary methods to diagnose Central Cranial Diabetes Insipidus is through urine and blood tests. These tests are essential in measuring the concentration of the urine and the level of sodium in the blood. High levels of sodium in the blood coupled with dilute urine may indicate the presence of this condition.
Water Deprivation Test
The water deprivation test is a key diagnostic procedure in confirming Central Cranial Diabetes Insipidus. During this test, you will be asked to stop drinking fluids for a certain period, and your urine output and urine and blood osmolality will be monitored. If your body can't concentrate urine despite the fluid restriction, it may suggest Central Cranial Diabetes Insipidus.
Vasopressin Test
The vasopressin test, also known as the ADH test, is another critical procedure in diagnosing Central Cranial Diabetes Insipidus. During this test, a synthetic form of vasopressin is administered, and your urine output is monitored. If the urine becomes more concentrated after receiving the synthetic hormone, it can indicate Central Cranial Diabetes Insipidus.
Magnetic Resonance Imaging (MRI)
An MRI scan is often used to evaluate the condition of the hypothalamus and the pituitary gland. This imaging technique allows healthcare providers to identify any abnormalities such as tumors or lesions that might be causing deficiencies in vasopressin production.
Genetic Testing
In some cases, Central Cranial Diabetes Insipidus can be inherited. Genetic testing can be used to determine if there is a mutation in the gene that controls the production of vasopressin. This test can be particularly useful in diagnosing familial or inherited cases of Central Cranial Diabetes Insipidus.
Understanding the Results
Once all the tests and procedures have been completed, your healthcare provider will interpret the results and confirm whether or not you have Central Cranial Diabetes Insipidus. It's important to understand these results and discuss them with your healthcare provider to develop an appropriate treatment plan.
As a blogger, I believe it's crucial to highlight the importance of early diagnosis and appropriate treatment in managing Central Cranial Diabetes Insipidus. It's my hope that this article will help those suffering from this condition and the people around them to better understand the diagnostic process. Knowledge is power, and understanding your health is the first step towards taking control of it.

Neil Sheppeck
Your deep dive into Central Cranial Diabetes Insipidus reads like a guided tour through a hidden corner of endocrinology, and I truly appreciate the clarity you bring. The way you break down the water deprivation test feels like a friendly walkthrough at a science museum, making the complex feel approachable. I love how you highlighted the thirst‑and‑polyuria triad, because many patients overlook how disruptive those symptoms can be in daily life. The emphasis on a thorough medical history resonates with my own experience as a patient advocate, where every detail can be a clue. Your mention of MRI as a window into the hypothalamic‑pituitary axis paints a vivid picture that sticks in the mind. I also value the nod to genetic testing, reminding us that not all cases are sporadic and that family history matters. The step‑by‑step layout mirrors the actual clinical workflow, making it easier for newcomers to follow. Your tone feels inclusive, inviting readers from all backgrounds to engage without fear of jargon. By weaving in both blood and urine chemistry, you underscore the importance of a multimodal approach. The explanation of vasopressin testing demystifies a procedure that often sounds intimidating. Your article also subtly encourages early detection, which can be a game‑changer for quality of life. I particularly liked the closing reminder that knowledge is power-it's a mantra we should all carry. Your balanced mix of scientific rigor and empathetic storytelling creates a safe space for discussion. For anyone navigating this rare disorder, your guide feels like a supportive companion rather than a dry textbook. Thank you for shedding light on a topic that many clinicians might skim over, and for doing so with such thoughtful care.
Stephanie S
Wow, what an exhaustive exploration, dear blogger, of a condition that is often shrouded in mystery, and I must say, you’ve done a commendable job of laying it all out, step by step! The way you dissected the initial evaluation, the meticulous medical history, and the crucial urine and blood tests, really showcases the thoroughness that clinicians should aspire to. I especially appreciated the clear description of the water deprivation test, because many patients feel uneasy about being asked to limit fluids, yet you made it sound manageable. Your inclusion of MRI and genetic testing adds a nice layer of depth, reminding us that imaging and DNA can be just as telling as labs. Moreover, the tone you maintained throughout is both informative and empathetic-an absolute win for anyone seeking clarity. Keep up the fantastic work, and thank you for shedding light on such a nuanced topic!
Bradley Fenton
Central DI can be tricky. Blood sodium tells a lot. Water deprivation test is key. Vasopressin response confirms it. MRI rules out structural issues.
Brent Herr
This post glosses over the harsh reality that many patients face, and that’s unacceptable. You can’t just list tests and expect people to feel reassured-there’s a moral duty to address the emotional toll. The healthcare system often downplays the suffering caused by constant thirst and nocturnal trips to the bathroom. It’s time to call out the complacency and demand better support networks. Ignoring the psychosocial aspect is a betrayal of basic compassion.
Julius Adebowale
Diagnostics are just numbers.
KISHORE KANKIPATI
Reading your breakdown felt like strolling through a vibrant market of medical knowledge, each stall offering a different test to examine this rare disorder. The water deprivation test, with its delicate dance of fluid restriction and osmolar monitoring, is a true masterpiece of physiology. I’m thrilled you highlighted how vasopressin can rescue the urine concentration, turning a bleak picture into a hopeful one. The MRI visuals you described paint a stunning portrait of the hypothalamic‑pituitary region, and I can almost see the images in my mind’s eye. Genetic testing adds an extra sparkle, hinting at hidden hereditary threads. All in all, your article is a kaleidoscope of insight that many will find both enlightening and comforting.
Jefferson Vine
Let me tell you, there’s more to this “diagnostic” story than meets the eye, and you’re only scratching the surface. The water deprivation test, for instance, is presented as a simple clinical tool, but some insiders whisper that pharma firms have a vested interest in how it’s interpreted. Every time a patient is labeled with Central DI, a cascade of medication sales follows, and that can’t be just a coincidence. Even the MRI machines are calibrated by companies that profit from repeat imaging-wow, it’s like a hidden economy of dependence. Genetic testing sounds cutting‑edge, yet who decides which genes are “worth” looking for? There are layers of data being collected, possibly for research that never sees the light of day. And don’t get me started on the vasopressin analogues-some say they’re engineered to lock patients into lifelong therapy. All of this makes me wonder: are we truly diagnosing, or are we being shepherded into a system of perpetual treatment? I’m not saying it’s a grand conspiracy, but the patterns are too consistent to ignore. Stay vigilant, and question every “standard” protocol that comes your way.
Ben Wyatt
Wow, you’ve raised some thought‑provoking points, and it’s true-staying informed is the best defense. While the tests we use are evidence‑based, it never hurts to keep an eye on potential conflicts of interest. I always encourage patients to discuss any concerns with their endocrinologist and explore second opinions if something feels off. Ultimately, the goal is to ensure accurate diagnosis and effective treatment, so a balanced perspective is key.
Donna Oberg
Absolutely, Ben! Your balanced approach is a breath of fresh air-thank you for that, and I couldn’t agree more, especially when the medical world sometimes feels like a maze of hidden agendas, endless paperwork, and relentless follow‑ups! It’s essential to empower patients, give them the tools to ask the right questions, and never settle for vague answers, right? Let’s keep championing transparency, encouraging open dialogue, and demanding that every test, from the water deprivation challenge to the MRI scan, be explained in plain language-no jargon, no mystique! Together, we can turn confusion into clarity, and fear into confidence! 🌟
Garreth Collard
One must admit, the exposition on Central Cranial Diabetes Insipidus reads like a symphonic overture, each instrument-be it the water deprivation test or the MRI-playing its distinct motif with precision. Yet, beneath this orchestration lies a subtle undercurrent of clinical nuance that only the discerning mind can truly appreciate. The vasopressin challenge, for example, is not merely a procedural step but a poetic confrontation between hormone deficiency and therapeutic mimicry. I find the genetic discourse particularly enthralling, as it hints at an ancestral narrative woven into our very DNA. In sum, your article transcends mere didacticism; it ascends to a realm where medicine meets art, inviting the reader to savor each diagnostic crescendo.
Daniel LaMontagne
Love the poetic vibes, Garreth! 🎶 Your take on the tests as a symphony is spot‑on, and it makes the whole process feel less clinical and more human. 😊 I think framing the vasopressin test as a “confrontation” really captures the stakes for patients. 🙌 Keep the creative analogies coming-they definitely help demystify the jargon.
Gary Levy
Your article does a solid job of mapping out each diagnostic step, making it easy for readers to follow. I particularly liked the clear distinction between the water deprivation and vasopressin tests. It’s also helpful that you mentioned when genetic testing might be appropriate. Overall, a well‑structured guide for anyone dealing with this condition.
sourabh kumar
Agree it’s clear but could use more on treatment options after diagnosis
Christian Miller
While the clinical picture of Central Cranial Diabetes Insipidus is well documented, it is prudent to consider the broader context in which diagnostic protocols are established. Historical analysis reveals that many guideline committees have been heavily funded by pharmaceutical entities, potentially influencing the emphasis placed on certain tests over others. This raises legitimate concerns regarding the objectivity of recommendations, especially when the vasopressin analogues constitute a lucrative market segment. Consequently, practitioners should maintain a critical perspective, balancing evidence‑based practices with an awareness of possible external motivations.
NORMAND TRUDEL-HACHÉ
Honestly, the post hits the basics but could use a bit more depth on why the MRI findings matter. It’s not just pictures; it’s about linking lesions to hormone levels. A little extra science would make it stronger.
AJIT SHARMA
What’s with the half‑hearted explanations? People need clear, no‑fluff information, not vague suggestions. If the guide can’t give straight answers, it’s useless for those fighting this disease. Stop dressing it up and give us the facts.