Opioid Constipation Management Calculator
Opioid-induced constipation affects nearly every person on long-term opioid therapy. This calculator helps determine the right laxative regimen based on your opioid type and treatment duration.
Recommended Regimen
No calculation yet. Enter your information above.
When opioids are prescribed for severe pain - after surgery, for cancer, or following a major injury - they work. But they also bring along a group of unwelcome guests: constipation, drowsiness, and nausea. These aren’t rare or unusual reactions. They’re expected. In fact, constipation happens in nearly every single person who takes opioids long-term. Drowsiness hits up to 60% of new users. Nausea affects about one in three. And if you’re not prepared for them, these side effects can make life harder than the pain you’re trying to treat.
Constipation: The Most Predictable Side Effect
Opioids don’t just slow down pain signals in your brain. They also slow down your gut. When these drugs bind to receptors in your intestines, they reduce the muscle movements that push food along. Fluid gets absorbed instead of being moved out. The result? Hard stools, bloating, and a feeling that you just can’t go - even when you really need to. This isn’t something that goes away after a few days. Unlike drowsiness or nausea, constipation sticks around as long as you’re on opioids. The American Academy of Family Physicians calls it the most common side effect of chronic opioid use. And they’re clear: don’t wait until you’re stuck. Start a laxative regimen on day one. The go-to combo? A stimulant laxative like senna to kickstart movement, plus an osmotic agent like polyethylene glycol to pull water into the colon. Drinking plenty of water helps, too. If that doesn’t cut it, there are targeted options like methylnaltrexone (Relistor) or naloxegol (Movantik). These drugs block opioid effects in the gut without touching the pain relief in your brain. They’re not cheap, but for people stuck for weeks, they’re life-changing.Drowsiness: When Your Brain Feels Like It’s Underwater
You take your opioid pill. Within an hour, you feel heavy. Your thoughts move slow. You zone out during conversations. You almost fall asleep driving home. This is opioid-induced sedation - and it’s common. About 20% to 60% of people feel this way when they first start opioids. The brain’s alertness centers get suppressed. Mental fog sets in. For many, it fades after a week or two as the body adjusts. But for 10% to 15% of long-term users, the drowsiness never fully lifts. That’s a problem when you’re trying to work, care for kids, or even just stay awake at the dinner table. The fix isn’t always more pills. First, try timing your dose. Take it at night if possible. Skip other sedating meds like benzodiazepines or alcohol - combining them increases the risk of dangerous breathing problems. If you’re still tired, talk to your doctor about lowering the dose. Sometimes, a smaller amount of a stronger opioid works better than a high dose of a weaker one. There’s some evidence that stimulants like methylphenidate (Ritalin) can help, but studies are thin. And they come with their own side effects - increased heart rate, anxiety, trouble sleeping. Don’t try to self-treat this. Work with your provider. Your brain needs time to adapt, but it shouldn’t be permanently foggy.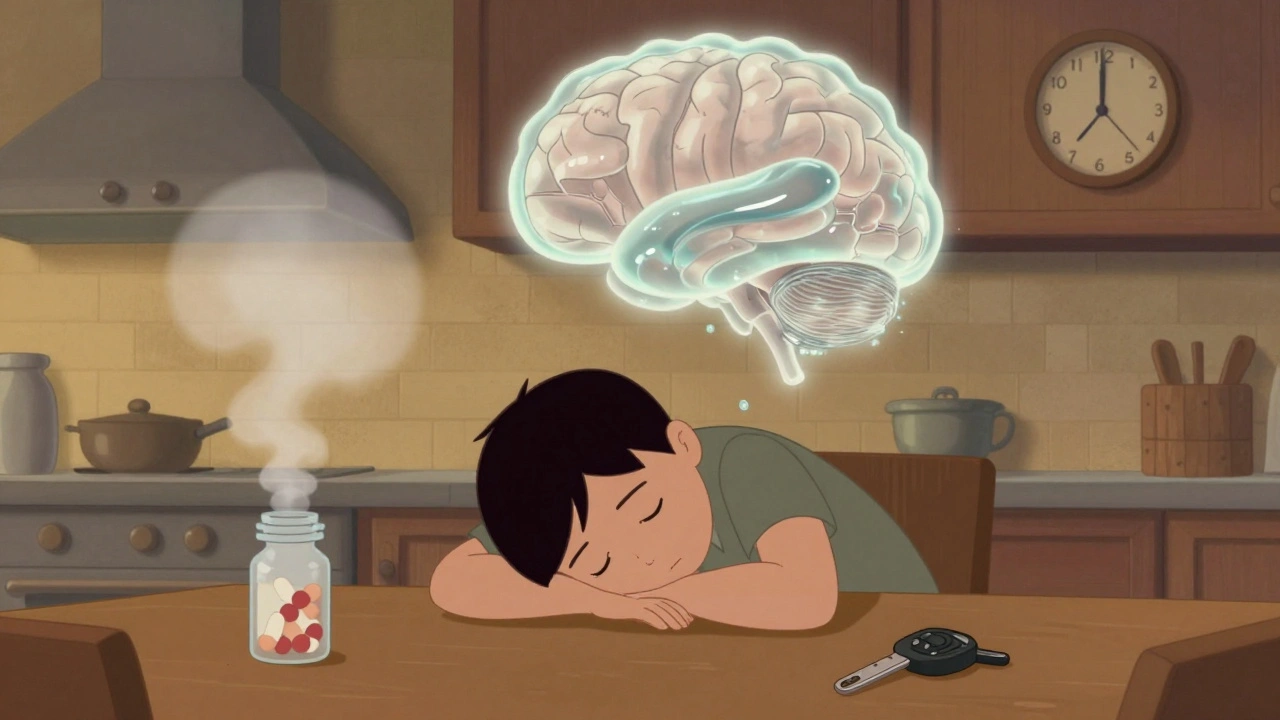
Nausea: Why Your Stomach Feels Like It’s Revolting
Nausea from opioids hits fast. It’s not just an upset stomach. It’s a signal from your brainstem. Opioids directly irritate the area that controls vomiting - the chemoreceptor trigger zone. They also slow down stomach emptying, so food sits there longer, making you feel queasy. About 25% to 30% of new users get nauseated. For most, it fades within 3 to 7 days. But for 1 in 10, it lingers. That’s enough to make someone skip doses or quit the medication entirely - even if they’re still in pain. Treatment depends on what’s causing it. If it’s brainstem irritation, dopamine blockers like metoclopramide or prochlorperazine often work best. If it’s slow digestion, domperidone (where available) helps. Ondansetron, a serotonin blocker, is great for chemo nausea but less reliable for opioids. Antihistamines like promethazine can help too, but they add more drowsiness - which might make things worse. Don’t just endure it. Ask your doctor for an antiemetic to start alongside your opioid. Sometimes, just switching from hydrocodone to oxycodone helps - different opioids have different nausea profiles. And never stop suddenly. Abruptly quitting opioids can cause a flood of nausea, vomiting, diarrhea, and sweating. That’s withdrawal - and it’s dangerous.Why Managing These Side Effects Matters More Than You Think
These three side effects aren’t just annoying. They’re roadblocks to safe, effective pain care. People who can’t manage constipation may stop taking their pain meds. That leads to uncontrolled pain - and sometimes, to seeking illegal drugs. The CDC found that more than two-thirds of people who misused prescription opioids did so to relieve physical pain. If your doctor doesn’t talk to you about constipation, drowsiness, and nausea upfront, you’re not getting full care. The FDA and CDC both warn that sudden opioid withdrawal can trigger severe symptoms - including vomiting, diarrhea, and spikes in blood pressure. That’s why tapering off must be slow and supervised. And if you’re on opioids long-term, you need a plan. Not just for pain, but for your gut, your alertness, and your stomach.
What You Can Do Right Now
- If you’re starting opioids: Ask for a bowel regimen - senna + polyethylene glycol - on day one.
- Take your dose at night if drowsiness is bad. Avoid driving or operating machinery until you know how you react.
- Keep a symptom journal: Note when nausea hits, how tired you feel, and how often you go to the bathroom. Bring it to your next appointment.
- Never mix opioids with alcohol, benzodiazepines, or sleep aids. The risk of fatal breathing problems jumps dramatically.
- If side effects are keeping you from living your life, speak up. There are alternatives - lower doses, different drugs, non-opioid pain options.
When to Call Your Doctor
- Constipation lasts more than 3 days despite laxatives
- You’re so drowsy you can’t stay awake during the day
- Nausea leads to vomiting more than once a day
- You feel confused, slow to respond, or have trouble breathing
- You want to stop the medication - don’t quit cold turkey
These aren’t signs you’re weak. They’re signs your body needs help adjusting. Good pain care means managing the whole picture - not just the pain.
Do opioid side effects go away over time?
Some do, some don’t. Drowsiness and nausea often improve within a week or two as your body builds tolerance. But constipation almost never goes away on its own. It requires ongoing management with laxatives or targeted medications. Don’t assume it’ll get better - plan for it from the start.
Can I take over-the-counter laxatives with opioids?
Yes, and you should. OTC stimulant laxatives like senna and osmotic agents like MiraLAX (polyethylene glycol) are safe and effective when used as directed. Many doctors recommend starting both together on day one of opioid therapy. Avoid stool softeners alone - they’re not strong enough for opioid-induced constipation.
Why do opioids make me feel sick but not others?
Everyone’s body reacts differently. Genetics, age, liver function, and even gut bacteria can influence how you respond. Older adults and people with prior nausea from other medications (like chemotherapy) are more likely to get sick. Some opioids, like codeine, are more nausea-prone than others. If one makes you nauseous, your doctor might switch you to a different one.
Is it safe to drive while taking opioids?
Not until you know how they affect you. Opioids can slow reaction time, blur vision, and cause drowsiness - even if you don’t feel sleepy. Studies show impairment similar to having a blood alcohol level of 0.05%. Wait at least a week after starting or increasing your dose. If you still feel foggy, don’t drive. It’s not worth the risk.
What happens if I stop opioids suddenly?
Stopping abruptly can cause severe withdrawal: nausea, vomiting, diarrhea, muscle aches, anxiety, and intense pain. The FDA warns this can lead to uncontrolled pain, psychological distress, or even suicide. Never quit cold turkey. Work with your doctor to taper slowly - often over weeks or months - to avoid these dangerous effects.


Ignacio Pacheco
So let me get this straight - we’re prescribing drugs that turn your gut into a concrete mold, make you nap through your kid’s soccer game, and turn your stomach into a war zone… and we call this ‘pain management’? Brilliant. Just brilliant.
parth pandya
yes u r right abt constipation its worst part i had to use miralax daily for 8 months after spine surgery and still felt bloated. doc said just drink water but bro water dont fix opioid gut 😅
Jim Schultz
Oh, for heaven’s sake - if you can’t handle the side effects of a class of drugs that literally shuts down your nervous system to numb pain, maybe you shouldn’t be on them in the first place? The fact that people treat constipation like a personal betrayal is absurd. It’s pharmacology, not a conspiracy. Senna? PEG? Of course they work - they’ve been around since the 1950s! Why are we acting like this is some newfangled mystery?!
And don’t even get me started on the ‘I feel foggy’ crowd. You’re on a Schedule II narcotic. Of course your cognition is impaired. You’re not ‘sick’ - you’re medicated. Get a grip.
Also - stop blaming the drug. Stop acting like your body is being ‘attacked.’ It’s not. It’s responding exactly as it’s supposed to. The gut has opioid receptors for a reason. You didn’t break your biology - you just didn’t read the damn manual.
And yes, I know someone who took methylnaltrexone for six months. It cost $12,000 a year. And guess what? They still complained. Because some people don’t want solutions - they want validation that their discomfort is a tragedy.
Let me guess - you also think caffeine makes you ‘anxious’ and that sunlight is ‘harsh on your skin’? There’s a pattern here. You’re not patients. You’re consumers who expect perfection from a system designed to manage suffering - not eliminate it.
Next time you’re tempted to tweet ‘opioids ruined my life,’ ask yourself: did the opioid ruin your life - or did you refuse to manage the inevitable?
And before you say ‘but my doctor never told me!’ - well, that’s your doctor’s fault. Not the drug’s. Not the system’s. Yours. You didn’t ask. You didn’t read. You didn’t prepare. And now you’re mad because reality didn’t bend for you?
Get a journal. Track your bowel movements. Talk to a pharmacist. Use the tools that exist. Stop treating every side effect like a personal affront.
And for God’s sake - stop mixing opioids with alcohol. You’re not a lab rat. You’re an adult. Act like one.
Albert Essel
I appreciate the thorough breakdown, especially the distinction between acute and chronic side effects. Many patients assume drowsiness will fade - and it often does - but constipation is the silent killer of adherence. I’ve seen patients discontinue opioids not because of pain, but because they couldn’t sit through a family dinner without feeling like they were about to explode. That’s not weakness. That’s physiology.
The recommendation to start laxatives on day one is gold. Too many providers wait until the patient is already in distress. Prevention is always better than crisis management - especially with something as predictable as opioid-induced constipation.
Also, the note about switching opioids based on nausea profile is underutilized. Oxycodone vs. hydrocodone vs. morphine - the differences in emetic potential are real. A simple switch can be life-changing without increasing risk.
And yes - never stop cold turkey. Withdrawal isn’t just uncomfortable; it’s a medical emergency. The body adapts. The nervous system rewires. Tapering isn’t optional. It’s non-negotiable.
Thank you for writing this. It’s the kind of information that should be handed out with every prescription.
Chloe Madison
Y’all need to stop acting like side effects are a failure. They’re not. They’re just part of the deal. I had a friend on long-term opioids after a car crash - she started senna and MiraLAX on day one, took her dose at night, kept a symptom log, and still went to work, played with her kids, and traveled. She didn’t ‘beat’ the side effects - she managed them. And that’s what this is: management. Not magic. Not punishment. Just smart care.
Also - if your doctor didn’t talk to you about this? Find a new one. This isn’t rocket science. It’s standard of care. You deserve better than silence.
Vincent Soldja
Constipation. Drowsiness. Nausea. All known. All expected. All manageable. Done.
Makenzie Keely
I’m so glad someone finally said this out loud - constipation isn’t just ‘a little uncomfortable,’ it’s a full-blown nightmare. I had a cousin who went 11 days without a bowel movement on oxycodone. She ended up in the ER. They gave her an enema. She cried the whole time. She wasn’t weak - she was unprepared. Please, if you’re starting opioids - ask for the bowel protocol. Don’t wait. Don’t hope. Ask. Now.
And if you’re a provider - stop assuming your patient knows. Hand them the pamphlet. Write it on the script. Say it twice. This is preventable suffering. We owe them that.
Katherine Gianelli
My grandma was on opioids after her hip replacement - and she didn’t say a word about the nausea until she started vomiting every morning. She thought it was just ‘old age.’ Turns out, it was the morphine. Her nurse gave her a tiny dose of promethazine and suddenly she was eating oatmeal again. No drama. No panic. Just a simple fix.
Don’t suffer in silence. Don’t think it’s ‘normal’ to feel like you’re going to die every time you eat. That’s not normal - that’s a side effect with a solution. Talk to someone. Anybody. A pharmacist, a nurse, a friend who’s been there. You’re not alone. And you don’t have to grin and bear it.
Also - your body isn’t broken. It’s just doing what it’s told. And you? You’re brave for even trying to manage this. That counts.
Joykrishna Banerjee
Let’s be honest - most people who complain about opioid side effects are just looking for an excuse to stop taking them because they’re addicted and don’t want to admit it. Constipation? You’re not ‘blocked,’ you’re just not using your bowels like a disciplined adult. Drowsiness? Maybe you’re just lazy. Nausea? Probably your junk food diet. The real issue isn’t the drug - it’s the entitlement. We’ve turned pain management into a luxury spa experience. It’s not. It’s medicine. Take it. Manage it. Stop whining.
Also - if you’re taking ‘natural remedies’ or ‘CBD oil’ instead of your prescribed dose, you’re not being ‘holistic’ - you’re being dangerous. Opioids are not optional. They’re life-saving. Stop romanticizing your suffering.
And for the love of God - stop posting about this on Reddit like it’s a TikTok trend. People die because of misinformation. Be responsible.
Francine Phillips
My husband took oxycodone after his back surgery. Constipation was brutal. We tried everything. Then we just started giving him prune juice every morning. Not fancy. Not expensive. Just worked. Sometimes the simple stuff is the best stuff.
Kidar Saleh
In the UK, we have a phrase: ‘It’s not the pain that breaks you - it’s the waiting.’ Waiting for relief. Waiting for a doctor. Waiting for the nausea to pass. But here’s the truth - the side effects of opioids are not a failure of the patient. They’re a failure of the system that treats them like an afterthought. If we treated constipation with the same urgency as pain, we’d have fewer people dropping out of care. Fewer people turning to street drugs. Fewer people dying in silence. This isn’t about individual weakness. It’s about institutional neglect. And it’s time we stopped pretending otherwise.
Albert Essel
Francine’s prune juice comment is spot-on. Sometimes the most effective interventions are the oldest ones. Prunes, water, movement - they’re not glamorous, but they’re evidence-based. I’ve seen patients reject ‘old-school’ advice because it sounds too simple. But simplicity isn’t weakness. It’s wisdom.
And to the person who said ‘just take it’ - you’re missing the point. People aren’t whining because they want to avoid pain. They’re frustrated because they were never told how to manage the side effects. That’s not entitlement. That’s a lack of education. And it’s on us - providers, patients, and systems - to fix it.