When your doctor orders a brain MRI, it’s not because they’re being overly cautious-it’s because they need to see what’s happening inside your skull in a way no other test can. Unlike CT scans or X-rays, MRI doesn’t use radiation. Instead, it uses strong magnets and radio waves to create detailed pictures of your brain’s soft tissues. This makes it the most powerful tool doctors have for spotting problems like strokes, tumors, multiple sclerosis, and even early signs of dementia. But what do those images actually show? And how do doctors tell the difference between normal aging and something serious?
What a Brain MRI Really Shows
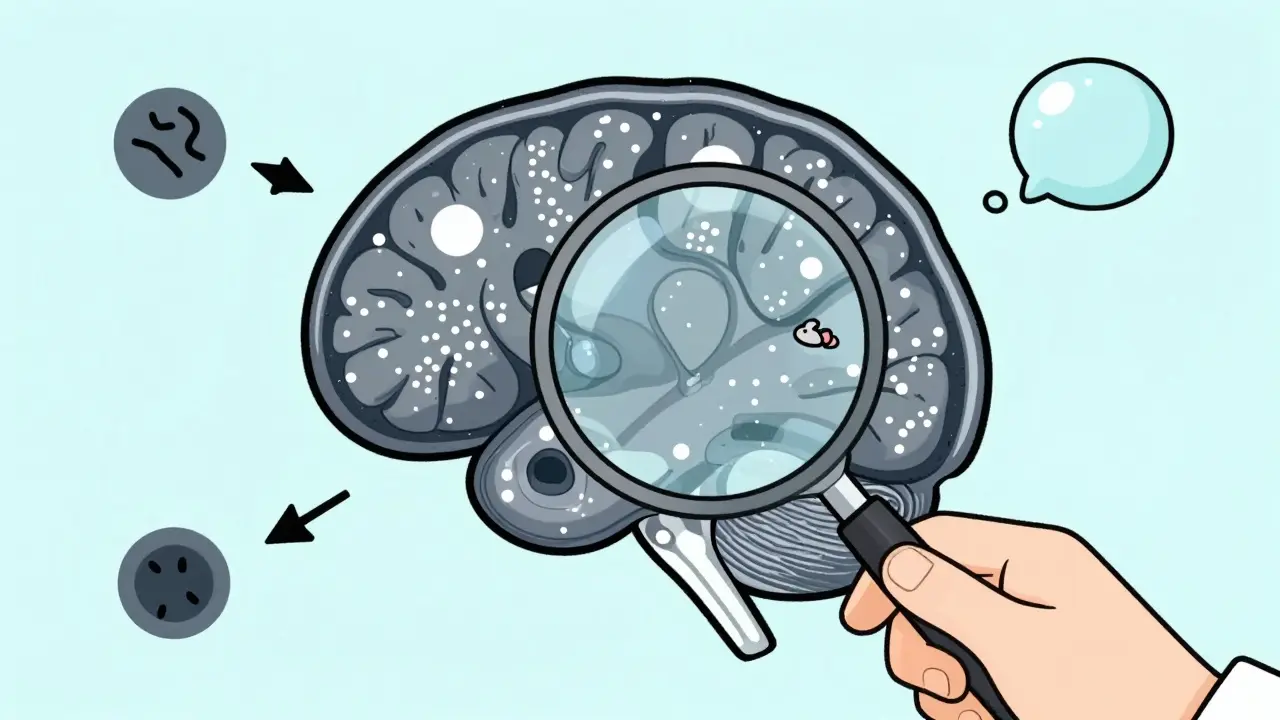
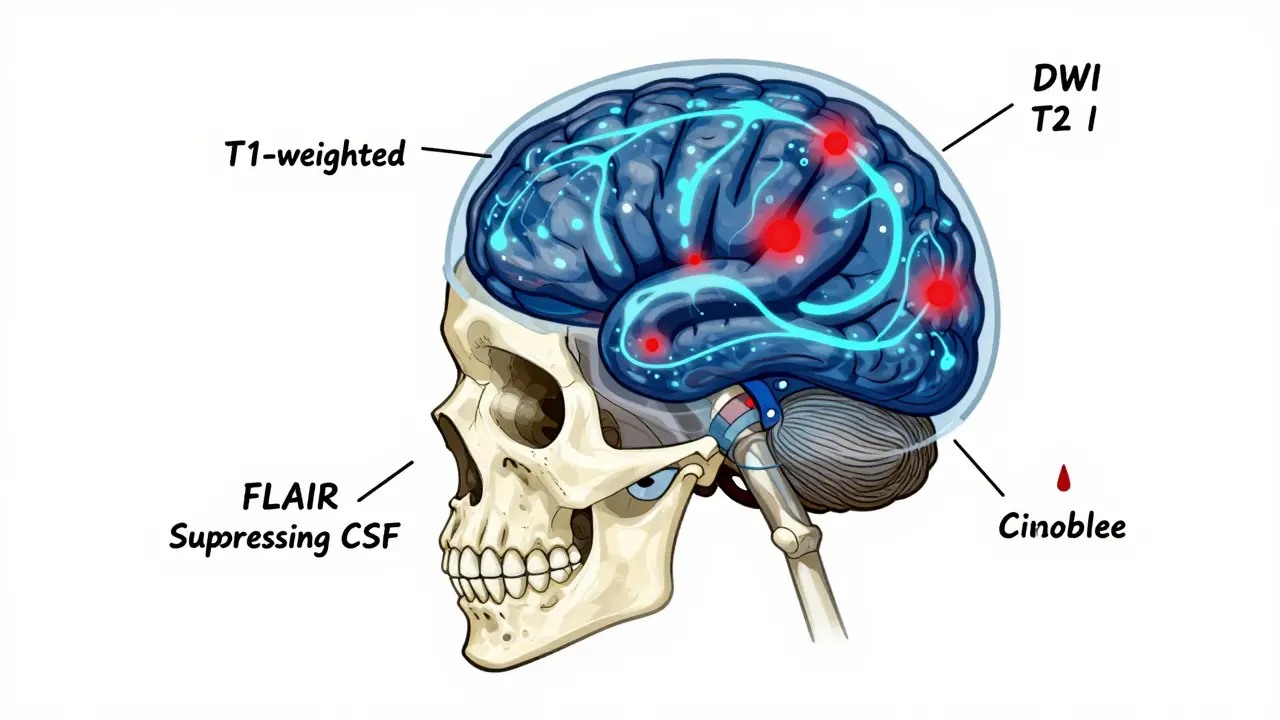
A brain MRI doesn’t just give you a picture-it gives you multiple pictures, each highlighting different things. These are called sequences, and each one reveals a different part of the story. The most common ones are T1-weighted, T2-weighted, FLAIR, DWI, and SWI.
T1-weighted images are like a detailed anatomy map. Fat and some types of tissue appear bright white, while fluid like cerebrospinal fluid (CSF) looks dark. This is great for seeing the brain’s structure-where the gray matter ends and white matter begins. It’s also the best view for spotting bleeding that’s been around for a while, or for checking if a tumor is pushing on nearby structures.
T2-weighted images, on the other hand, make water shine bright. That means swelling, inflammation, and most types of damage show up clearly. But here’s the catch: CSF also looks bright on T2, so it can be hard to tell if a bright spot near the ventricles is a lesion-or just fluid. That’s where FLAIR comes in.
FLAIR (Fluid-Attenuated Inversion Recovery) is like T2, but with one smart trick: it turns CSF dark. Now, anything bright on FLAIR that’s not CSF? That’s abnormal. This is the go-to sequence for spotting multiple sclerosis plaques, small strokes, or infections near the brain’s surface. A bright spot next to a ventricle on FLAIR? That’s a red flag. A bright spot on T2 but dark on FLAIR? Probably just CSF.
Diffusion-weighted imaging (DWI) is the emergency responder. It picks up strokes within minutes-long before a CT scan can. When brain cells die from lack of oxygen, water can’t move the way it should. DWI catches that. If the numbers (ADC values) drop below 600 x 10^-6 mm²/s, it’s an acute stroke. This one change can mean the difference between full recovery and permanent disability.
SWI (Susceptibility-Weighted Imaging) finds tiny bits of blood you’d never see otherwise. It’s sensitive enough to catch microbleeds from high blood pressure, brain trauma, or even rare conditions like cerebral amyloid angiopathy. A few dots the size of a grain of salt? On SWI, they’re unmistakable.
Common Findings-and What They Mean
Not every bright spot on an MRI is a crisis. Many are normal, especially as we age.
White matter hyperintensities-those small bright patches near the ventricles-are seen in 15% of people under 50 and up to 90% of those over 70. They’re often linked to tiny blood vessel changes from high blood pressure or aging. Alone, they don’t mean dementia. But if they’re widespread, along with memory loss or slow thinking, they might point to vascular cognitive impairment.
Multiple sclerosis plaques are different. They’re usually oval-shaped, perpendicular to the ventricles, and show up clearly on FLAIR. They’re often found in the corpus callosum, brainstem, or spinal cord. A single lesion doesn’t confirm MS-it’s the pattern, the timing, and other tests that matter.
Small strokes, called lacunar infarcts, show up as tiny (3-5mm) bright spots in the basal ganglia, thalamus, or brainstem. These are silent in many people-no symptoms at all. But if you have more than five, your risk of future stroke or dementia goes up.
Brain tumors? They often appear as irregular masses with swelling around them. On T1 with contrast, they light up like a beacon because the blood-brain barrier is broken. But not all tumors glow-some are slow-growing and don’t enhance. That’s why follow-up scans are often needed.
And then there’s atrophy. When the brain shrinks, the ventricles get bigger. That’s normal with age, but if it’s faster than expected-especially in the hippocampus-it can signal Alzheimer’s. Doctors compare the size of brain structures to age-matched norms. A 65-year-old with the brain volume of an 80-year-old? That’s a red flag.
Why MRI Beats CT for Most Neurological Issues
CT scans are fast. In an emergency room, they’re the first line. But for anything beyond trauma or acute bleeding, MRI wins. It shows 100 times better contrast between gray and white matter. It sees the back of the brain-the cerebellum and brainstem-without bone blocking the view. CT can miss small tumors, early strokes, or MS plaques entirely.
Take acoustic neuromas-tiny, non-cancerous tumors on the hearing nerve. CT might miss anything under 5mm. MRI picks up ones as small as 2mm. That’s why anyone with sudden hearing loss or ringing in one ear gets an MRI, not a CT.
And for multiple sclerosis? MRI finds 97% of lesions. CT finds 65%. That’s a huge gap.
But MRI isn’t perfect. It takes 30 to 45 minutes. You have to lie still. It’s loud. And if you have a pacemaker, cochlear implant, or certain metal fragments, you can’t have one. In trauma cases, speed matters more than detail. That’s why CT still rules the ER.
What MRI Can’t Tell You
Here’s something many patients don’t realize: an MRI shows structure, not function. It can show a lesion, but not whether it’s causing your headache, dizziness, or memory lapse.
That’s why doctors don’t order MRIs for every headache. In fact, the American College of Radiology says MRI is usually not appropriate for uncomplicated migraines. Studies show only 1.3% of brain MRIs done for routine headaches reveal anything serious. Most people with migraines have perfectly normal scans.
Also, MRI can’t tell you how old a lesion is-not without contrast or special sequences. A bright spot could be from a stroke last week, or one from ten years ago. That’s why your history matters. Did the symptoms start suddenly? Are they getting worse? That context turns a picture into a diagnosis.
How Radiologists Read an MRI-Step by Step
It’s not random. Experienced radiologists follow a strict order:
- Start with the midline. Is the brain centered? Are the ventricles symmetrical?
- Check the ventricles and CSF spaces. Are they enlarged? Is there any blockage?
- Look at the basal ganglia and thalamus. Any small bright spots? Those could be old silent strokes.
- Scan the white matter. Are there FLAIR hyperintensities? Are they in the right pattern?
- Examine the cortex and lobes. Any swelling? Any asymmetry?
- Check the cerebellopontine angles. That’s where acoustic neuromas hide.
- Look at the meninges and skull base. Any abnormal enhancement?
One common mistake beginners make? Mistaking blood vessels for lesions. Flow voids-dark spots where blood rushes through-are normal. But if you’re new to reading MRIs, they can look like holes in the brain. That’s why training takes 6 to 12 months.
What’s New in Brain MRI?
Technology is moving fast. 7.0T MRI machines-seven times stronger than standard hospital scanners-are now in 23 U.S. research centers. They can show individual layers of the cortex, something never seen before. This could change how we understand epilepsy and Alzheimer’s.
Artificial intelligence is cutting scan times in half. Software like Quantib can automatically detect brain atrophy, tumors, or MS lesions, helping radiologists spot things faster and with fewer errors.
And then there’s diffusion tensor imaging (DTI). It doesn’t just show where lesions are-it maps the brain’s wiring. It shows how nerve fibers connect different regions. In multiple sclerosis, it can show damage to white matter tracts even before lesions appear.
By 2027, doctors may routinely use quantitative MRI-measuring actual numbers like myelin content or blood flow-instead of just looking at pictures. That’s the future: not just seeing the problem, but measuring it.
When to Worry-and When Not To
Let’s be real: most people who get a brain MRI don’t have a tumor or MS. Most have normal scans. Even when there’s a finding, it’s often harmless.
If you have:
- Sudden, severe headache (thunderclap)
- Weakness on one side
- Loss of vision or speech
- Seizures
- Progressive memory loss with personality changes
-then an MRI is essential.
If you have:
- Chronic migraines with no neurological symptoms
- Occasional dizziness with no other signs
- Forgetfulness that doesn’t interfere with daily life
-then an MRI is unlikely to help, and may even cause unnecessary stress.
The goal isn’t to find every tiny anomaly. It’s to find the things that matter-and rule out the dangerous ones.
Is a brain MRI dangerous?
No, brain MRI is not dangerous. It doesn’t use radiation. The magnetic field is strong, but it’s not harmful. The main risks come from metal implants-pacemakers, cochlear implants, or certain types of surgical clips-that could move or heat up. If you have any metal in your body, tell your doctor before the scan. Claustrophobia is also common; many centers offer open MRI machines or sedation if needed.
How long does a brain MRI take?
A standard brain MRI takes between 30 and 45 minutes. High-resolution scans, like those for the inner ear or pituitary gland, can take longer-up to 60 minutes. You’ll need to lie still. Movement blurs the images. Some scans require contrast dye, which adds 10-15 minutes. You’ll hear loud knocking sounds-earplugs are provided.
Can MRI detect Alzheimer’s disease?
MRI can’t diagnose Alzheimer’s on its own, but it can show signs that support the diagnosis. The most common finding is shrinkage (atrophy) in the hippocampus and temporal lobes. In advanced cases, the whole brain may appear smaller. While PET scans that detect amyloid plaques are more specific, MRI is widely used because it’s more available and shows structural changes early.
Why do I need contrast dye for some MRIs?
Contrast dye (gadolinium) helps highlight areas where the blood-brain barrier is broken-like tumors, infections, or active MS plaques. Without contrast, some lesions blend in with normal tissue. Contrast makes them stand out. It’s safe for most people, but those with severe kidney disease may need special precautions. The dye leaves your body through urine within 24 hours.
Are white spots on my MRI normal?
Small white spots on MRI, called white matter hyperintensities, are common-especially as you get older. They’re often due to tiny blood vessel changes from high blood pressure or aging. If they’re few and scattered, they’re usually not a problem. But if they’re large, numerous, or in unusual places, they might suggest MS, vascular disease, or another condition. Your doctor will compare them to your symptoms and other tests.
Can MRI miss a brain tumor?
MRI is the best tool for finding brain tumors, but it’s not perfect. Very small tumors, especially if they don’t disrupt the blood-brain barrier, might not show up clearly without contrast. Some slow-growing tumors look like normal tissue. That’s why follow-up scans are sometimes needed. If symptoms persist despite a normal MRI, further testing or repeat imaging may be recommended.
What Comes Next After Your MRI?
If your MRI is normal, and your symptoms are mild, your doctor may suggest monitoring or lifestyle changes-like controlling blood pressure, getting more sleep, or reducing stress. No news can be good news.
If there’s a finding, your doctor will explain what it means in context. One lesion? Maybe nothing. Multiple lesions with neurological symptoms? That’s a different story. Sometimes, you’ll need another test-like a spinal tap, EEG, or blood work-to confirm a diagnosis.
Don’t rush to Google your results. Radiologists use years of training to interpret these images. A single finding can mean ten different things. What matters most is your overall picture: your symptoms, your history, your physical exam.
Brain MRI is a window into the most complex organ in your body. It doesn’t give all the answers-but it gives the clearest view we have. And that’s why it remains the gold standard.

Jamie Hooper
so i got my MRI last week and they found these 'white matter hyperintensities'... honestly i thought i was gonna die. turns out it's just my brain aging like a bad cheese? thanks for the clarity, doc. 🙃
Husain Atther
This is an exceptionally well-structured overview of brain MRI interpretation. The distinction between FLAIR and T2 sequences is particularly illuminating for non-specialists. Such clarity in medical communication is rare and deeply appreciated.
Izzy Hadala
I'm curious about the statistical validity of the 97% lesion detection rate for MS via MRI versus CT. Could you provide the source study? The methodology behind such a significant disparity would be valuable to examine, particularly regarding sensitivity thresholds and sample size.
Vatsal Patel
oh so the brain is just a wet sponge now? white spots = old age? wow. next they'll tell me my liver is just a 'fatty memory stick'. they got me on MRI so they can sell me more meds. classic. 🤡
Sharon Biggins
this was soo helpful!! i was stressing over my MRI results but now i get it. white matter stuff is common, right? like, not a death sentence? thank you for explaining it like i'm not a doctor lol 💕
John McGuirk
they say MRI is safe but what about the EMF? they're scanning your brain with magnets stronger than a train engine. what if it's rewiring your thoughts? what if they're tracking you? i heard the military uses this tech to mess with veterans. you think they told you that?
Michael Camilleri
people get scared over white spots but they never think about what they ate that day or if they're just lazy. your brain shrinks because you watch tiktok all day not because of some invisible disease. take responsibility. stop blaming your MRI
lorraine england
i love how you broke this down! my dad had an MRI last year and i was so lost. now i can actually talk to him about his results without feeling like i'm speaking alien. you made this feel human 😊
Darren Links
in america we spend billions on MRIs while other countries fix their water supply. this is what happens when profit drives medicine. why not just give people vitamin D and sunshine? but nooo, we gotta scan their brains for $3000.
Kevin Waters
This is such a solid breakdown. I'm a neurotech engineer and I appreciate how you explained DWI and ADC values in plain terms. I've had patients ask me the same questions - this is exactly what I wish I could hand them. Great job.
Kat Peterson
OMG I just got my MRI results and I have a 'lesion' 😭 I thought I was gonna die. like, i'm only 28? this is so unfair. why is my brain betraying me?? 😭💔 #brainanxiety #mrihellscape
Himanshu Singh
The brain is not just a machine. It's a symphony of energy, memory, and silent stories. MRI captures the echo, not the song. We focus on spots and forget the silence between them. Maybe the real diagnosis is how afraid we are of not knowing.
Helen Leite
i heard the MRI machine can see your soul?? like... if you're a bad person it shows dark spots?? my cousin said her mom's scan showed a black hole near her heart and they said 'it's not physical'... i'm scared to get one now 😵💫
Karen Conlin
Thank you for this. I've mentored patients through MRI results for over a decade, and this is one of the clearest summaries I've seen. Especially the part about not overinterpreting white matter changes. So many people panic over normal aging. You've given them peace of mind. 🙌
asa MNG
so i read this whole thing and then my wife said 'you're just stressed'... so i went to the ER and demanded an MRI. they said i didn't need one. now i'm convinced they're hiding something. my brain feels different. like... quieter. like they turned off a channel. i know what i feel. 😤