SSRI Bleeding Risk Calculator
Assess Your Bleeding Risk
This tool estimates your bleeding risk based on the SSRI you're taking and your health factors. Based on clinical studies and guidelines.
Your Bleeding Risk Assessment
Important Considerations
Remember: This tool provides an estimate based on published data. Your actual risk may vary.
Always consult your healthcare provider for personalized medical advice.
When you take an SSRI for depression or anxiety, you’re not just changing your mood-you’re also affecting how your blood clots. It’s not a side effect most people talk about, but it’s real, measurable, and sometimes dangerous. Selective Serotonin Reuptake Inhibitors (SSRIs) like fluoxetine, sertraline, and paroxetine are among the most prescribed antidepressants in the world. But behind their mood-lifting benefits lies a quiet, often overlooked risk: bleeding.
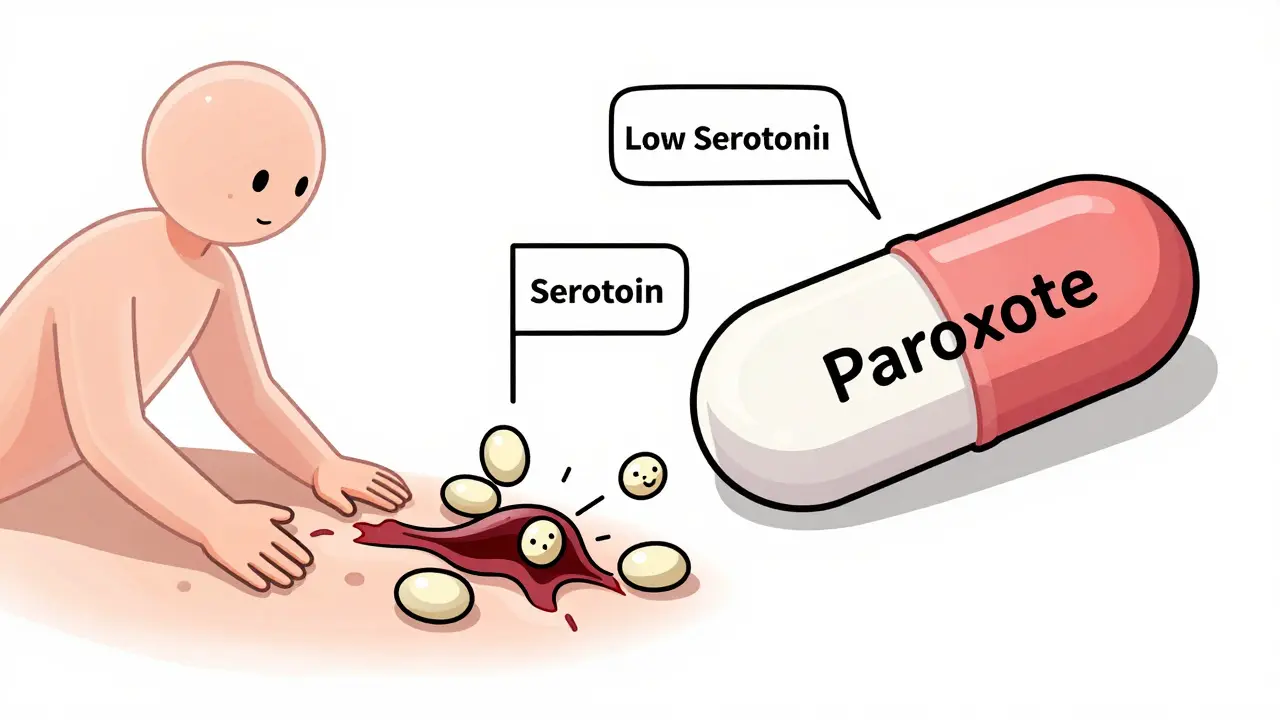
Why SSRIs Make You Bleed More Easily
Platelets are the tiny blood cells that rush to a cut to form a clot. They need serotonin to work properly. Here’s the catch: platelets don’t make serotonin. They steal it from the blood, storing up to 99% of the body’s total serotonin inside them. That serotonin acts like a signal-when a blood vessel gets damaged, platelets release it to attract more platelets and lock the clot in place. SSRIs block the serotonin transporter (5-HTT), the same protein platelets use to suck up serotonin from the blood. When that transporter is blocked, platelets run low on serotonin. No serotonin means weaker signals. Weaker signals mean slower, less effective clots. The result? You bruise more easily. A paper cut takes longer to stop bleeding. You might notice nosebleeds after blowing your nose too hard. This isn’t theory. Studies show that people on paroxetine-one of the strongest SSRIs at blocking serotonin uptake-have over 80% less serotonin in their platelets. That’s not a small drop. That’s a functional impairment. The more the drug blocks serotonin reuptake, the worse the platelet dysfunction. Paroxetine and fluvoxamine are the worst offenders. Sertraline and citalopram? Much milder.Not All SSRIs Are Equal When It Comes to Bleeding
This is where things get practical. If you’re on an SSRI and worried about bleeding, not all drugs are created equal. The key is how tightly each one binds to the serotonin transporter. That’s measured by something called Ki value-the lower the number, the stronger the binding, and the higher the bleeding risk.- Paroxetine: Ki = 0.17 nM → Highest bleeding risk
- Fluvoxamine: Ki = 0.34 nM → High risk
- Sertraline: Ki = 0.52 nM → Moderate risk
- Citalopram: Ki = 0.91 nM → Lower risk
When SSRIs Combine With Other Drugs, Risk Skyrockets
The real danger isn’t just SSRIs alone. It’s what happens when they mix with other medications that also thin the blood. Take blood thinners like warfarin or apixaban. Add an SSRI on top? Your risk of major bleeding jumps by 35%, according to a 2024 JAMA Network Open study. That’s not a small increase. That’s enough to send someone to the ER. NSAIDs like ibuprofen or naproxen? Even worse. When taken with SSRIs, the bleeding risk goes up 4.5 times. That’s because NSAIDs damage the stomach lining and reduce clotting factors. Combine that with serotonin-starved platelets? You’re asking for trouble. Even antiplatelet drugs like aspirin or clopidogrel add to the problem. But here’s a surprising twist: a 2023 study found that patients on SSRIs who also got prasugrel or ticagrelor (stronger antiplatelets used after heart stents) didn’t bleed more than those not on SSRIs. Why? Because those drugs work so hard to block platelets anyway that adding an SSRI doesn’t make much difference. It’s like pouring water into a flooded basement-it doesn’t change the level.
Who’s Most at Risk?
Not everyone on SSRIs will bleed. But some people are sitting on a ticking clock.- People over 65
- Those with a history of ulcers or GI bleeding
- Patients with kidney or liver disease
- Anyone on anticoagulants or NSAIDs
- People with genetic variants in the serotonin transporter gene (5-HTTLPR S/S genotype)
What to Do Before Surgery or Dental Work
If you’re scheduled for surgery, a colonoscopy, or even a tooth extraction, your doctor needs to know you’re on an SSRI. For procedures with high bleeding risk, guidelines suggest stopping the SSRI 5 to 7 days beforehand. But here’s the catch: stopping antidepressants suddenly can trigger withdrawal or make depression worse. The American Psychiatric Association says: don’t stop SSRIs for heart surgery. The risk of depression relapse after cardiac procedures is higher than the bleeding risk. But for a wisdom tooth removal? That’s different. Talk to your doctor. Don’t assume it’s safe to keep taking it. Some hospitals now use platelet-rich plasma during surgery to help SSRI patients clot better. A 2023 study showed it cut bleeding time by over 40%. It’s not standard yet-but it’s being tested.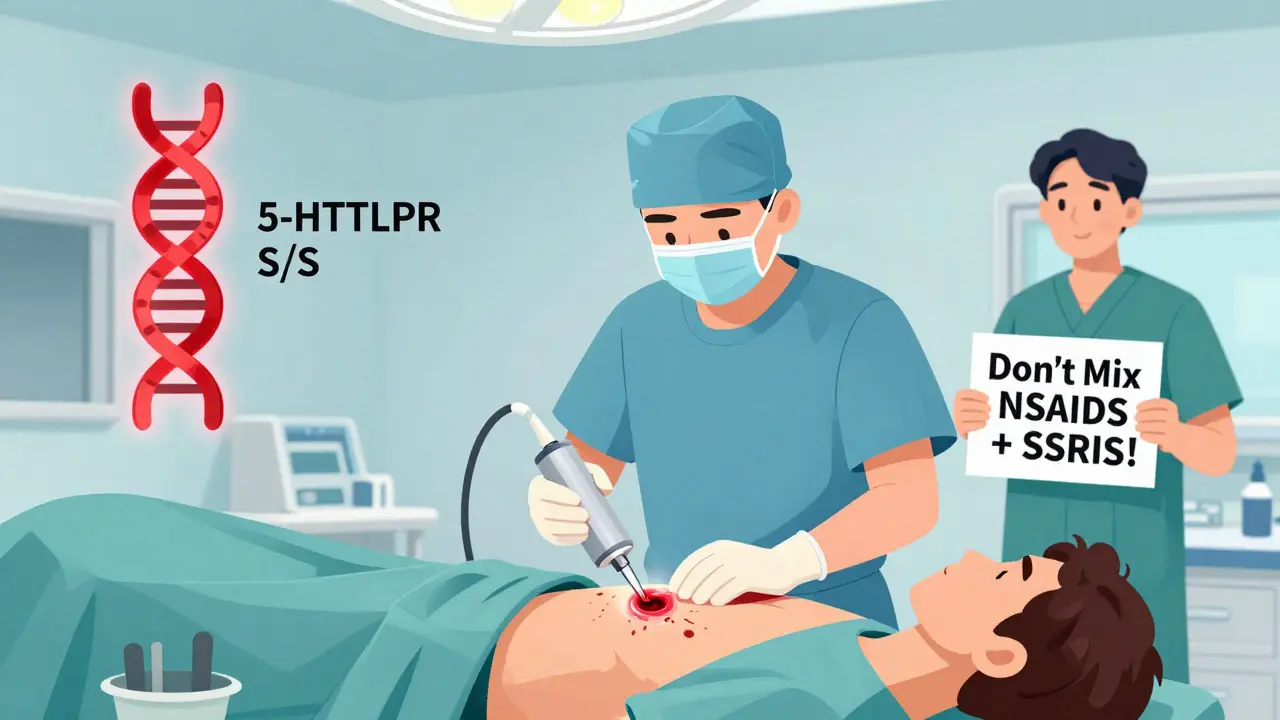
Genetics Might Soon Tell You Your Risk
Your genes might hold the answer. The 5-HTTLPR gene controls how many serotonin transporters your body makes. People with two short versions (S/S genotype) have fewer transporters. When they take an SSRI, their platelets get even emptier of serotonin. A 2024 study found these people had 2.3 times the bleeding risk compared to those with two long versions (L/L). The European Medicines Agency is reviewing whether to add genetic testing to SSRI labels by late 2025. If approved, doctors might test your gene before prescribing. That could mean avoiding paroxetine entirely if you’re S/S. It’s personal medicine in action.What You Should Watch For
You don’t need to panic. But you do need to be aware. Here’s what to look out for:- Unexplained bruising, especially large or painful ones
- Nosebleeds that last longer than 10 minutes
- Bleeding gums when brushing or flossing
- Passing black, tarry stools or red blood in stool
- Vomiting material that looks like coffee grounds
- Unusual prolonged bleeding from cuts
What’s the Bottom Line?
SSRIs save lives. Untreated depression increases your risk of heart disease, suicide, and early death. You shouldn’t stop taking them just because of bleeding risk. But you should know your risk level.- If you’re on paroxetine or fluvoxamine and have other risk factors, talk to your doctor about switching.
- Never take NSAIDs with SSRIs unless your doctor says it’s safe.
- Always tell every doctor and dentist you’re on an SSRI before any procedure.
- For high-risk patients, sertraline or citalopram are safer choices.
- Genetic testing might soon help guide your choice-but it’s not routine yet.
Do all SSRIs cause bleeding?
No. Bleeding risk varies by SSRI. Paroxetine and fluvoxamine carry the highest risk because they strongly block serotonin uptake in platelets. Sertraline and citalopram have much lower binding affinity and are safer choices for people at risk of bleeding.
Can I take ibuprofen with an SSRI?
Avoid it. Combining NSAIDs like ibuprofen or naproxen with SSRIs increases bleeding risk by 4.5 times. Use acetaminophen (Tylenol) for pain instead, unless your doctor says otherwise.
Should I stop my SSRI before surgery?
It depends. For minor procedures like dental work, stopping 5-7 days before may be advised. For major surgeries like heart surgery, guidelines recommend continuing SSRIs because depression relapse poses a greater threat than bleeding risk. Always consult your doctor-don’t stop on your own.
Is sertraline safer than paroxetine for bleeding risk?
Yes. Sertraline has a much lower binding affinity for the serotonin transporter than paroxetine. Studies show paroxetine users have 40-50% higher risk of GI bleeding compared to sertraline users. For patients with bleeding risk factors, sertraline is the preferred SSRI.
Can genetic testing tell me if I’m at higher risk?
Emerging evidence says yes. People with the S/S genotype of the 5-HTTLPR gene have 2.3 times higher bleeding risk on SSRIs than those with L/L. While not yet standard practice, the European Medicines Agency may require genetic risk stratification on SSRI labels by late 2025.
What are the signs of serious bleeding from SSRIs?
Watch for black or tarry stools, vomiting blood or material that looks like coffee grounds, unexplained large bruises, nosebleeds lasting more than 10 minutes, or bleeding that won’t stop after minor injuries. These require immediate medical attention.

Erwin Kodiat
Man, I never thought about how SSRIs mess with platelets. I’ve been on sertraline for years and just assumed my random bruises were from being clumsy. Turns out I got lucky with the drug choice.
Thanks for laying this out so clearly.
Lydia H.
It’s wild how a drug meant to fix your mind can quietly mess with your blood. We talk about mental health like it’s separate from the body, but it’s all connected. This post is a quiet wake-up call.
Maybe we need more doctors who think like this.
Astha Jain
OMG I’m on paroxitine and I’ve been bleeding from my gums for months 😭 I thought it was just bad flossing. Time to switch ASAP. Thanks for the heads up!!
Lewis Yeaple
While the data presented is largely accurate, it is important to note that the absolute risk of clinically significant bleeding remains low in healthy individuals without comorbidities. The relative risk increases are meaningful, but population-level implications must be contextualized against the benefits of effective antidepressant therapy.
Overreaction to pharmacovigilance signals without risk stratification may lead to undertreatment of depression, which carries its own mortality burden.
Jackson Doughart
This is one of those posts that makes you pause. I’ve seen patients on paroxetine develop GI bleeds after just a few weeks on NSAIDs. No one connects the dots until it’s too late.
It’s not the SSRI alone-it’s the cocktail. And most patients don’t even know they’re mixing fire with gasoline.
Doctors need to be better at explaining this. Patients deserve to know.
Jake Rudin
...And yet, the fact that serotonin is not synthesized by platelets, but rather sequestered from plasma via the SERT transporter... is the critical mechanistic insight here. Without this, the entire pharmacological cascade collapses. The Ki values? Valid. The clinical correlations? Robust. But the root cause? It’s all about transporter saturation... and the fact that platelets are essentially serotonin sponges with no internal production capacity...
Which is why fluvoxamine, despite its lower Ki than paroxetine, still causes significant dysfunction-because it’s dosed higher...
And don’t get me started on CYP2D6 polymorphisms affecting metabolism...
It’s not just the drug-it’s the person.
Josh Kenna
Bro, I took ibuprofen for a headache last week and ended up in the ER with a GI bleed. They asked if I was on antidepressants. I said ‘sertraline.’ They said ‘oh thank god it’s not paroxetine.’ I didn’t even know that was a thing. I’m switching tomorrow. This is life-or-death info and no one talks about it.
Thanks for posting this. I’ve been telling my friends to read it.
Valerie DeLoach
As someone who’s worked in primary care for 18 years, I’ve seen this pattern over and over. Patients come in with unexplained bruising, and we blame aging or vitamin deficiency. We never ask about their antidepressant. This is a systemic blind spot.
Let’s make this part of routine med reconciliation. Every time a patient fills an SSRI script, we should print a one-pager on bleeding risks and alternatives.
It’s not just about prescribing-it’s about educating. And we’re failing.
Christi Steinbeck
Stop scrolling. Read this. Save someone’s life. I’ve lost two friends to GI bleeds-both on paroxetine and ibuprofen. One was 32. Both thought it was ‘just a side effect.’
Switching to sertraline saved my cousin’s life. Don’t wait for a hospital visit to learn this. Talk to your doctor. Now.
Jacob Hill
...And if you’re over 65, or have a history of ulcers, or take aspirin for your heart... this isn’t just ‘something to consider’-it’s a red flag. Please, please, please don’t ignore this. I’ve seen too many people get told ‘it’s just bruising’ until they’re in the OR.
Knowledge is power. Share this.
Malikah Rajap
Wait… so if I’m S/S genotype, and I’m on paroxetine, and I take ibuprofen, and I’m 70… am I basically a walking time bomb? 😅
Also, is this why my grandma kept getting nosebleeds after her Zoloft? She never told anyone. I’m so mad I didn’t know this sooner.
sujit paul
Pharmaceutical companies knew this for decades. They suppressed the data because SSRIs are too profitable. The FDA is complicit. Genetic testing? A distraction. The real solution is to ban SSRIs entirely and return to therapy, sunlight, and natural serotonin boosters like exercise and omega-3s. This is chemical enslavement disguised as medicine.
Tracy Howard
Can we just acknowledge that Americans are overmedicated? We treat every mood swing with a pill, then act shocked when the pill starts bleeding people from the inside. In Canada, we use talk therapy first. SSRIs are a last resort. Maybe we’re doing something right.