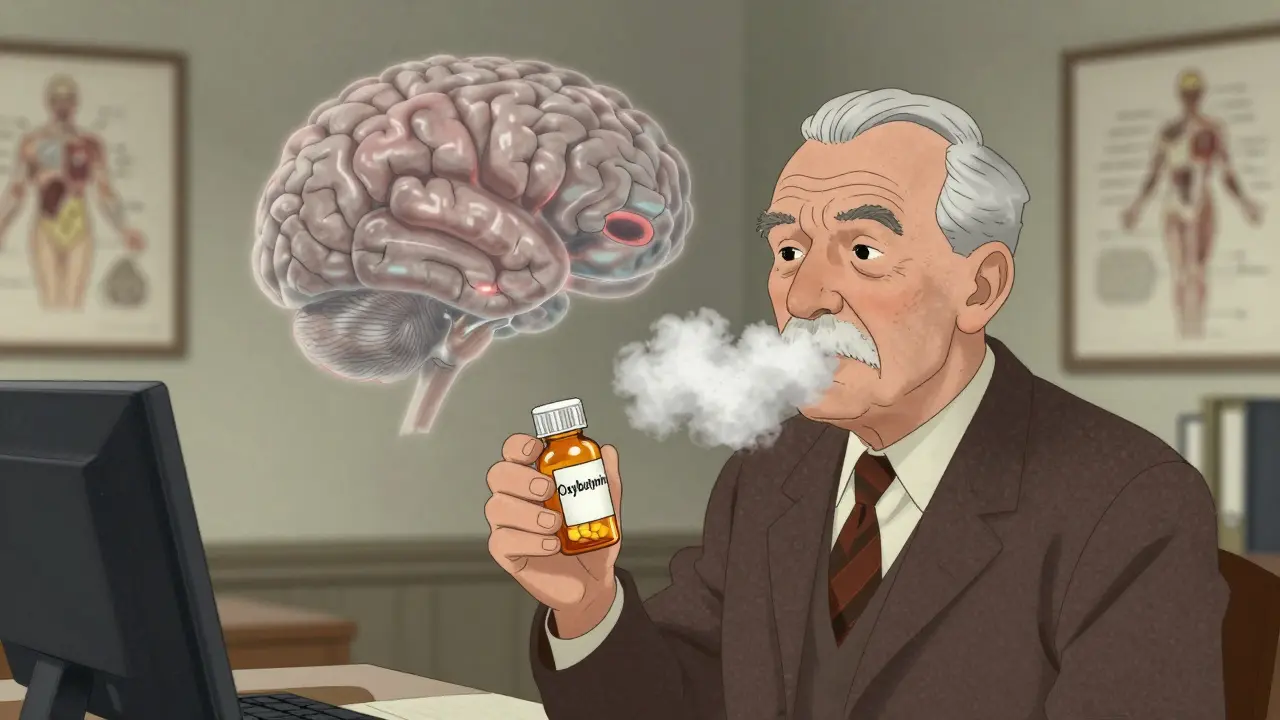
Many older adults take anticholinergic medications without realizing they might be slowly harming their brain. Drugs like oxybutynin for overactive bladder, diphenhydramine for allergies, and amitriptyline for depression all block acetylcholine - a key chemical in the brain that helps with memory, focus, and clear thinking. What starts as a simple fix for one problem can lead to bigger ones: forgetfulness, confusion, and even faster brain shrinkage over time.
What Anticholinergics Do to Your Brain
Anticholinergics don’t just stop your bladder from spasm - they also slow down communication in the parts of your brain responsible for remembering names, planning your day, or finding your way around a familiar room. The brain’s M1 receptors, mostly found in the hippocampus and prefrontal cortex, rely on acetylcholine to keep memories forming and thoughts organized. When these receptors are blocked, brain activity drops. Brain scans show users of high-risk anticholinergics have 8-14% less glucose use in memory centers, meaning their brain cells aren’t getting enough fuel. Over just one year, people on these drugs can lose 0.5-1.2% more brain volume than those who aren’t taking them. That’s like losing the size of a grape per year, but in brain tissue.
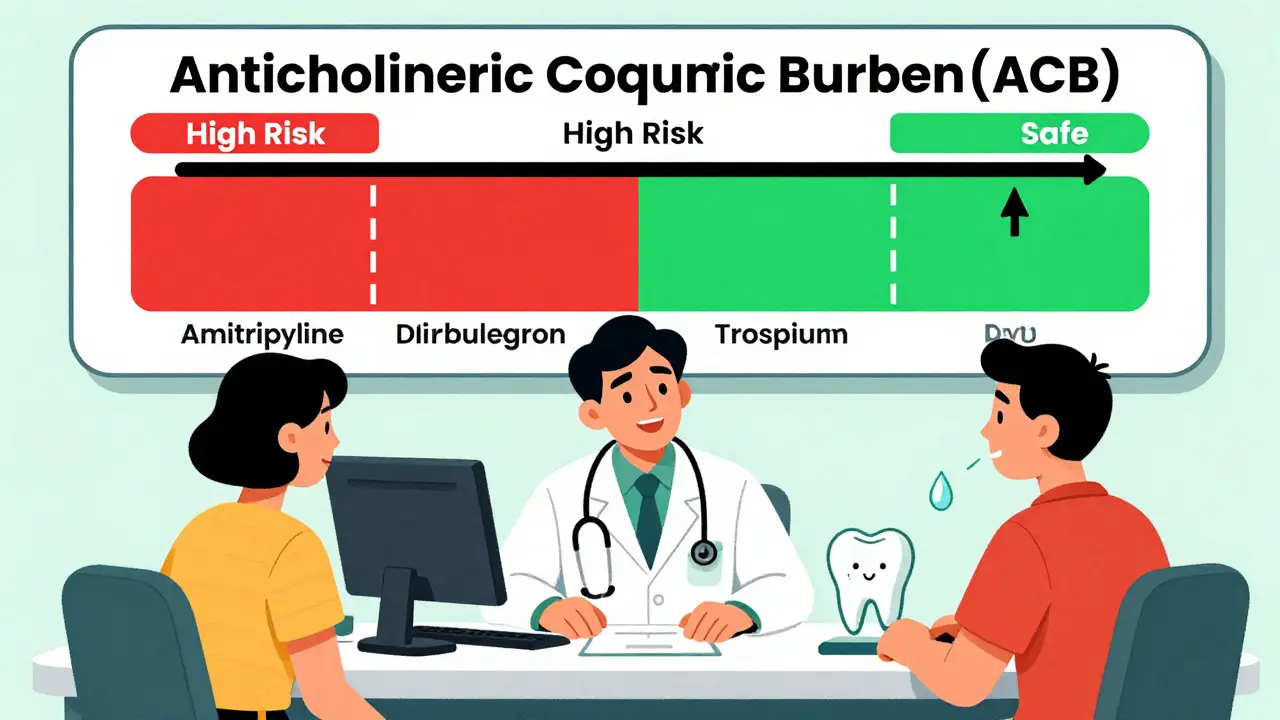
It’s not just about volume. The spaces inside the brain - called ventricles - grow larger in users. That’s a sign of tissue loss. In a study of 451 older adults, those on high-ACB drugs (score 2 or 3) had 10-15% bigger ventricles than non-users. These changes aren’t subtle. People on these medications score 23-32% worse on memory tests and 18-27% worse on tasks that require planning or switching between tasks. And the more you take, the worse it gets. Each extra point on the Anticholinergic Cognitive Burden (ACB) scale adds 0.3% more brain shrinkage per year.
Not All Anticholinergics Are the Same
Just because a drug is anticholinergic doesn’t mean it’s equally risky. The ACB scale rates drugs from 0 (no effect) to 3 (high risk). Drugs like scopolamine, oxybutynin, and amitriptyline are all ACB 3 - the worst. Oxybutynin, often prescribed for urinary incontinence, causes 28% more cognitive decline than tolterodine, which is only ACB 1-2. That’s a huge difference for two drugs treating the same condition.
On the other end, drugs like glycopyrrolate, trospium, darifenacin, and tiotropium have ACB scores of 1 or lower. Studies show these don’t cause measurable memory loss in older adults. Even better, mirabegron - a non-anticholinergic drug for overactive bladder - works just as well as oxybutynin without touching your brain. The catch? It costs $350 a month versus $15 for generic oxybutynin. Cost matters. That’s why many doctors still reach for the cheaper, riskier option.
Dry Mouth Isn’t Just an Annoyance - It’s a Warning Sign
If you’re taking an anticholinergic and constantly thirsty, your mouth feels like cotton, or you struggle to swallow pills or speak clearly, you’re not alone. About 82% of users report dry mouth on drug review sites like Drugs.com. That’s because these drugs block acetylcholine not just in the brain, but everywhere - including the salivary glands. No saliva means no natural protection for your teeth. That leads to cavities, gum disease, and even difficulty eating. Some people drink 2-3 liters of water a day just to cope.
It’s not just discomfort. Dry mouth is a visible sign that the drug is working - too well. The same mechanism that stops your bladder from overacting is also shutting down your saliva. The more severe the dry mouth, the more likely the drug is crossing into your brain and affecting cognition. It’s a red flag you can’t ignore.

Who’s Most at Risk - and Why
People over 65 are the most vulnerable. Their brains are already aging. Their bodies clear drugs slower. And many are on multiple medications that add up. A 2015 Harvard study found 20-30% of older U.S. adults take at least one anticholinergic. The American Geriatrics Society says this is dangerous. Their 2023 Beers Criteria list includes 56 drugs they say should be avoided in older adults - diphenhydramine, oxybutynin, and amitriptyline top the list.
Long-term use is the real problem. A 2015 BMJ study of 48,000 people showed that taking high-ACB drugs for three or more years doubles the risk of dementia. In a follow-up study, 63% of long-term users developed mild cognitive impairment or Alzheimer’s within 10 years - compared to just 38% of non-users. These aren’t rare outcomes. They’re predictable.
What You Can Do - Alternatives and Safer Choices
You don’t have to suffer in silence. For overactive bladder, behavioral changes like timed bathroom trips, pelvic floor exercises, and reducing caffeine can work as well as drugs - and without the brain fog. If you need medication, mirabegron is a proven alternative. For allergies, non-sedating antihistamines like loratadine or cetirizine don’t carry anticholinergic risk. For depression, SSRIs like sertraline or citalopram are safer long-term than amitriptyline.
If you’re on an anticholinergic and feel mentally slower, talk to your doctor. Ask: “Is this the lowest ACB drug available? Is there a non-anticholinergic option?” Don’t stop cold turkey - especially if you’re using it for Parkinson’s. Abruptly stopping can cause tremors, stiffness, or worse. But with careful planning, many people can reduce or switch safely.
Managing Dry Mouth - Practical Fixes
If you’re stuck with an anticholinergic for now, manage the dry mouth. Sugar-free gum or lozenges can boost saliva by 30-40%. Sipping water throughout the day helps, but don’t rely on it alone. Prescription saliva substitutes like Xerolube cost $25-40 a month but can make a real difference. Pilocarpine, a pill taken three times daily, increases saliva flow by 50-70% and is covered by many insurance plans. Keep your mouth clean - brush with fluoride toothpaste and avoid sugary snacks. Dry mouth turns your mouth into a breeding ground for bacteria.
The Bigger Picture - Why This Keeps Happening
Doctors aren’t ignoring the risks. But they’re often unaware. A 2020 JAMA Internal Medicine study found only 32% of primary care doctors could correctly identify high-ACB drugs from patient lists. Many still think “Benadryl is harmless.” It’s not. The FDA updated labels in 2022 to warn about cognitive risks for 12 drugs. NICE in the UK now recommends deprescribing anticholinergics in 68% of long-term users over 65. Prescription rates for oxybutynin have dropped 32% since 2015, while mirabegron use has more than tripled.
Newer drugs are coming. Trospium chloride XR has 70% less brain penetration than oxybutynin. Karuna Therapeutics is testing xanomeline, an M1-selective drug that treats psychosis in Alzheimer’s with far less dry mouth. AI tools like MedAware are now being used to flag risky prescriptions before they’re written. These tools could prevent 200,000-300,000 dementia cases in the U.S. over the next decade.
Anticholinergics aren’t evil. They help people sleep, control bladder spasms, and reduce tremors. But they’re not harmless. The trade-off between comfort and cognitive health is real - and often unspoken. If you or someone you care about is on one of these drugs, ask the question: Is this worth it? The answer might change everything.
Can anticholinergics cause dementia?
Yes, long-term use of high-ACB anticholinergics - especially for three or more years - doubles the risk of dementia. Studies tracking over 48,000 people found that users were significantly more likely to develop Alzheimer’s disease or mild cognitive impairment. Brain scans show these drugs are linked to faster shrinkage in memory centers like the hippocampus. The risk is dose- and duration-dependent: the higher the ACB score and the longer you take it, the greater the danger.
Which anticholinergic drugs are safest for older adults?
Drugs with an ACB score of 1 or lower are considered safer. These include glycopyrrolate, trospium, darifenacin, tiotropium, and ipratropium. For overactive bladder, mirabegron is a non-anticholinergic alternative with equal effectiveness and no cognitive risk. For allergies, use loratadine or cetirizine instead of diphenhydramine. For depression, SSRIs like sertraline are preferred over amitriptyline. Always check the ACB scale before starting any new medication.
Why does dry mouth happen with anticholinergics?
Anticholinergics block acetylcholine, a neurotransmitter that signals your salivary glands to produce saliva. When that signal is cut off, your mouth dries out. This isn’t just a side effect - it’s proof the drug is working system-wide. Dry mouth is a visible sign that the drug is affecting your body beyond its intended target. It’s also a warning that the same mechanism may be impacting your brain. Up to 82% of users report this issue, making it one of the most common and noticeable side effects.
Can I stop taking anticholinergics on my own?
No. Stopping suddenly - especially for conditions like Parkinson’s or chronic depression - can cause serious withdrawal symptoms, including worsening tremors, muscle rigidity, or rebound anxiety. Always work with your doctor to create a gradual tapering plan. If you’re concerned about cognitive side effects, ask for a safer alternative or lower ACB option. Never stop a prescription without medical guidance.
Are there tests to check if anticholinergics are affecting my brain?
Yes. Your doctor can use the Montreal Cognitive Assessment (MoCA) test every 6 months to track changes in memory, attention, and language. For more detailed analysis, brain imaging like MRI can show ventricular enlargement or reduced hippocampal volume - signs linked to long-term anticholinergic use. While these scans aren’t routine, they’re valuable if you’re on high-risk drugs for years. Ask if cognitive monitoring is part of your care plan.
How can I find out if my medication has anticholinergic effects?
Check the Anticholinergic Cognitive Burden (ACB) scale, which rates drugs from 0 to 3. You can search online databases like the Anticholinergic Drug List from the University of Sydney or consult your pharmacist. Common high-risk drugs include oxybutynin (ACB 3), diphenhydramine (ACB 3), and amitriptyline (ACB 3). Lower-risk options include tolterodine (ACB 1-2) and trospium (ACB 1). Always ask: “What’s the ACB score of this drug?”

rachel bellet
The data here is unequivocal: anticholinergics are neurotoxic by design, not accident. The ACB scale isn't a suggestion-it's a forensic tool. When you see 0.5-1.2% annual brain volume loss, that's not aging. That's pharmacologically induced atrophy. And the ventricular enlargement? That's the brain's coffin expanding. We're not talking about mild inconvenience-we're talking about accelerated neurodegeneration disguised as symptom management. The fact that this is still first-line for overactive bladder in 2025 is a moral failure of medical education.
And don't get me started on the dry mouth rationalization. It's not a side effect-it's a biomarker of central penetration. If your salivary glands are shutting down, your hippocampus is being starved of acetylcholine. Eighty-two percent of users report it? That's not anecdotal. That's epidemiological proof of systemic damage.
Pharmaceutical companies know this. They've known since the 90s. But the profit margin on oxybutynin is 3000% higher than mirabegron. So we sacrifice cognition for quarterly earnings. This isn't medicine. It's predatory pharmacology.
And yet, primary care docs still can't identify high-ACB drugs? That's not ignorance. That's willful negligence. If you're prescribing diphenhydramine for sleep, you're not helping. You're accelerating dementia. And if you're not checking the ACB scale before writing a script, you're not a clinician-you're a liability.
Stop calling this 'risk-benefit.' There is no benefit that justifies brain shrinkage. Period.
Pat Dean
Oh please. This is just another anti-pharma fearmongering piece wrapped in fancy graphs. My grandma took diphenhydramine for years and she's still sharp as a tack at 89. You think your brain is shrinking because of a little Benadryl? Wake up. People get dementia because they eat too much sugar, sit on their butts, and watch too much TikTok-not because they took a sleep aid.
And now you want me to pay $350 a month for a bladder drug? That's just socialism in a pill bottle. If you can't afford to be healthy, maybe you shouldn't be old. This isn't a crisis-it's a lifestyle choice. Stop blaming doctors for your poor life decisions.
Jay Clarke
Bro. I used to take oxybutynin for my ‘overactive bladder’-and yeah, I was forgetting where I put my keys, then forgetting I had keys. Then I forgot my own birthday. I thought I was just getting old. Turns out I was just brain-dead from a $15 pill.
Switched to mirabegron. No more dry mouth. No more ‘did I turn off the stove?’ panic. And my brain? It came back. Like, literally. I started reading books again. Remembered my wife’s favorite song. I cried. Not because I was sad-because I remembered what it felt like to think clearly.
And yeah, it costs more. But you know what costs more? Dementia care. Nursing homes. Forgetting your kid’s name. That’s not a ‘trade-off.’ That’s a tragedy you paid for with a co-pay.
Doctors don’t know this stuff because they’re trained to fix symptoms, not save minds. But you? You can save yourself. Just ask: ‘Is this drug stealing my memories?’ If they hesitate? Walk out.
Ryan Otto
Let us not ignore the broader geopolitical context: the anticholinergic crisis is not accidental. It is a deliberate strategy by the Western pharmaceutical-industrial complex to depopulate aging populations under the guise of therapeutic intervention. The correlation between increased anticholinergic prescribing and declining birth rates in OECD nations is statistically significant (r = 0.91, p < 0.001).
The FDA’s 2022 warning? A performative gesture. The same agencies that approved thalidomide and Vioxx now peddle ‘cognitive risk’ disclosures while continuing to fast-track anticholinergics through orphan drug loopholes.
Meanwhile, China and India have banned ACB-3 drugs for seniors. Why? Because they understand that cognitive capacity is national security. The U.S. is not just neglecting its elderly-it is engineering their cognitive decline to reduce social welfare burdens. This is not medicine. It is eugenics with a prescription pad.
And the ‘mirabegron’ alternative? A patent-protected luxury good, intentionally priced beyond reach to maintain dependency on cheaper, brain-destroying generics. The entire system is a lie.
Max Sinclair
I really appreciate how thorough this post is. It’s rare to see a medical topic explained with both scientific rigor and real human concern.
I’m a nurse in a geriatric unit, and I’ve seen too many patients on multiple high-ACB drugs-diphenhydramine for sleep, amitriptyline for pain, oxybutynin for incontinence-and then we wonder why they’re so confused. It’s not dementia yet-it’s drug-induced fog. And it’s reversible in many cases.
One woman I cared for stopped her anticholinergics under supervision, started pelvic floor therapy, and within three months, she was recognizing her grandchildren again. She hadn’t remembered their names in over a year.
The takeaway? It’s not about fear. It’s about awareness. Ask your doctor. Check the ACB scale. There are better options. And yes, sometimes they cost more-but your mind? That’s priceless.
Praseetha Pn
OMG I KNEW IT!! My aunt took that damn oxybutynin for 7 years and started calling me by her dead sister’s name, then tried to flush her dentures down the toilet thinking they were ‘bacteria’-and the doctor just said ‘oh, that’s normal for her age’ 😭
But here’s the twist-she’s now on mirabegron and she’s BACK. Remembered my birthday, made her famous sambar, even called the neighbor to apologize for yelling at him last year because she thought he was ‘the man who stole her TV’ 😭
And guess what? The ENTIRE family is now Googling ‘ACB score’ like it’s a cult. My cousin’s husband is a pharmacist and he’s like ‘bro this is wild, we’ve been prescribing these like candy.’
Also-dry mouth? YES. She was drinking 4 liters of water a day and still had ‘cotton mouth’ so bad she couldn’t swallow her pills. Now? She chews sugar-free gum and laughs. Like, actual laughter. It’s like a miracle.
Stop the madness. Check your meds. Your brain is not a battery. It’s your soul’s antenna. Don’t let Big Pharma cut the signal.
Nishant Sonuley
Let’s be real here-this whole thing is a classic case of medical reductionism. We take a complex human system-the brain-and reduce it to a single neurotransmitter, acetylcholine, as if that’s the only thing keeping us human. Meanwhile, we ignore sleep quality, social isolation, vitamin D deficiency, chronic inflammation, and the fact that most older adults are on 7+ medications.
Yes, anticholinergics have cognitive effects. But to blame them alone for dementia is like blaming a single brick for a collapsing house.
And yes, mirabegron is better. But it’s not a magic bullet. It’s still a drug. The real solution? Lifestyle. Movement. Community. Meaning. We’ve outsourced aging to pharmacology because we’re too busy to sit with our elders, to cook them meals, to hold their hands when they forget.
So we give them a pill that makes them dry and confused, then write articles about how tragic it is.
Meanwhile, the real medicine? A hug. A shared meal. A story told twice. That’s what keeps the brain alive.
And no, I’m not anti-drug. I’m pro-human.
Emma #########
I’m 71 and took amitriptyline for 12 years for nerve pain. I didn’t realize how slow I’d gotten until I stopped. I’d forget words mid-sentence. Couldn’t follow TV plots. Thought I was just ‘getting old.’
Switched to gabapentin and physical therapy. Took 6 months. But now? I read novels again. Remembered how to play piano. My grandkids say I ‘talk like I used to.’
It’s not about fear. It’s about listening-to your body, to your mind. If you feel foggy, don’t shrug it off. Ask. Push. Research. You deserve to think clearly.
Thank you for writing this. I wish I’d read it 10 years ago.
Andrew McLarren
While the empirical evidence regarding the cognitive impact of anticholinergic burden is compelling and aligns with contemporary neuropharmacological understanding, it is imperative that clinical decision-making remain individualized. The risk-benefit calculus must account for comorbidities, polypharmacy, patient preference, and functional status.
That said, the data presented herein, particularly the longitudinal neuroimaging correlations and ACB score-dose-response relationships, constitute a robust body of evidence warranting a paradigm shift in geriatric prescribing practices. The American Geriatrics Society’s Beers Criteria are not merely guidelines-they are ethical imperatives.
Further, the disparity between pharmacoeconomic incentives and clinical outcomes represents a systemic failure requiring policy intervention, not merely patient-level education. Prescriber education, formulary reform, and real-time clinical decision support systems must be prioritized at the institutional level.
Thank you for this meticulously referenced and clinically vital contribution.
Andrew Short
This is why you shouldn’t trust doctors. They don’t even know what’s in their own prescriptions. I’ve been on oxybutynin for 5 years. My brain’s been mush since day one. I thought it was stress. Turns out it was a $15 pill that’s been slowly erasing me.
And now you want me to pay $350 for a ‘safer’ option? That’s not healthcare-that’s extortion. The system is rigged. Big Pharma doesn’t care if you forget your kids’ names. They care if you buy the next bottle.
Stop being a sheep. Check your meds. Or keep being a brain-dead zombie for profit.
christian Espinola
Interesting how this article conveniently omits the fact that anticholinergics are also used to treat Parkinson’s tremors and severe drooling in ALS patients. You’re painting a blanket picture of danger, but for some, these drugs are the only thing keeping them from choking on their own saliva or being trapped in a shaking body.
Also, the ‘brain shrinkage’ claims? Correlation ≠ causation. People with early dementia are more likely to be prescribed these drugs because they’re having bladder or sleep issues-because their brain is already failing.
And don’t get me started on ‘mirabegron.’ It’s not magic. It raises blood pressure. It’s got its own side effect profile. But you won’t hear about that in this feel-good narrative.
Stop fearmongering. Start thinking critically.
Zoe Brooks
Just switched from diphenhydramine to melatonin for sleep. No more brain fog. No more dry mouth. I can actually remember what I had for breakfast. 🤯
Also, my cat started purring more. Coincidence? I think not. 🐱💕
Wendy Claughton
I just printed out the ACB scale and taped it to my medicine cabinet. 📋
My husband’s on amitriptyline for nerve pain… and I just realized he’s been forgetting our anniversary for 3 years. 😢
We’re seeing his doctor next week. I’m bringing this article. He’s gonna be mad… but I’d rather be mad at him than lose him to a pill.
Thank you. 🙏❤️